Thu, Apr 25, 2024
Volume 32, Issue 2 (3-2022)
JHNM 2022, 32(2): 89-97 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghaffari Sardasht F, Irani M, Mirzaii Najmabadi K, Nosrati Hadiababd S F, Fasanghari M. Breast Cancer Screening Behaviors Based on Health Belief Model. JHNM 2022; 32 (2) :89-97
URL: http://hnmj.gums.ac.ir/article-1-1827-en.html
URL: http://hnmj.gums.ac.ir/article-1-1827-en.html
Fatemeh Ghaffari Sardasht1 

 , Morvarid Irani *
, Morvarid Irani * 

 2, Khadijeh Mirzaii Najmabadi3
2, Khadijeh Mirzaii Najmabadi3 

 , Seyedeh Fatemeh Nosrati Hadiababd4
, Seyedeh Fatemeh Nosrati Hadiababd4 

 , Maryam Fasanghari4
, Maryam Fasanghari4 




 , Morvarid Irani *
, Morvarid Irani * 

 2, Khadijeh Mirzaii Najmabadi3
2, Khadijeh Mirzaii Najmabadi3 

 , Seyedeh Fatemeh Nosrati Hadiababd4
, Seyedeh Fatemeh Nosrati Hadiababd4 

 , Maryam Fasanghari4
, Maryam Fasanghari4 


1- PhD student of Reproductive Health, Student Research Committee, School of Nursing and Midwifery, Shahroud University of Medical Sciences, Shahroud, Iran b) Department of Midwifery, School of Nursing and Midwifery, Mashhad University of Medical Sciences, Mashhad, Iran
2- Department of Midwifery, School of Nursing and Midwifery, Torbat Heydariyeh University of Medical Sciences, Torbat Heydariyeh, Iran b) Health Sciences Research Center, Torbat Heydariyeh University of Medical Sciences, TorbatHeydariyeh, Iran , Irani.morvarid@gmail.com
3- Associated Professor, Nursing and Midwifery Care Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
4- Midwifery (MSc), school of nursing and midwifery, medical sciences university, Mashhad, Iran
2- Department of Midwifery, School of Nursing and Midwifery, Torbat Heydariyeh University of Medical Sciences, Torbat Heydariyeh, Iran b) Health Sciences Research Center, Torbat Heydariyeh University of Medical Sciences, TorbatHeydariyeh, Iran , Irani.morvarid@gmail.com
3- Associated Professor, Nursing and Midwifery Care Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
4- Midwifery (MSc), school of nursing and midwifery, medical sciences university, Mashhad, Iran
Full-Text [PDF 522 kb]
(512 Downloads)
| Abstract (HTML) (999 Views)
Full-Text: (527 Views)
Introduction
In 2020, 2.3 million women were diagnosed with breast cancer, and 685000 of them died globally. As of the end of 2020, there were 7.8 million women alive who have been diagnosed with breast cancer in the past 5 years, making it the world’s most prevalent cancer. There are more lost disability-adjusted life years by women due to breast cancer globally than any other type of cancer [1]. According to an estimate in 2020, the greatest cancer-related mortality will be observed in developing countries. In contrast, disease burden will reduce in Western countries due to the healthy lifestyle and better health facilities [2]. In Iran, breast cancer has been identified as the most common cancer and the fifth leading cause of death among Iranian women. The standardized incidence rate is about 28 per 100000 people, which has increased in recent years [3].
Every year, millions of cancer patients could be saved from premature death and suffering if they had timely access to early detection and treatment [4]. Survival for breast cancer is generally good, particularly if it is diagnosed early [5]. The most effective early detection methods are breast self-examination, mammography, and clinical breast examinations by physicians and healthcare professionals [6]. Breast cancer mortality is reduced by 40% in women aged 40-74 years who participate in screening every 1-2 years [7]. Breast self-examination can help detect 10% of breast cancer cases, especially in younger women who did not undergo mammography [8]. Secondary prevention through monthly breast self-examination is the best option to tackle the rising incidence of breast cancer [9]. A study has shown that age, level of education, information about breast cancer, family history of cancer, and understanding the importance of screening are influential factors in performing breast cancer self-examination [10]. Another breast cancer screening method is the clinical breast examination by a physician. About two-thirds of the reduction in breast cancer mortality could be attributed to clinical breast examination [11].
In the study of Tuyen, 15.8% of women underwent clinical breast examination [12]. Mammography is one of the best screening methods. This method is an early and timely diagnosis of breast cancer before it reaches a diameter of 5 mm [13]. Use of mammography in women under 50 with timely diagnosis and treatment of cancer results in a 5-year relative survival rate of around 90% [14]. According to the investigations, despite the availability of appropriate, accessible, and low-cost screening programs for all individuals, public acceptance of using these facilities is negligible [15]. In the Alharbi study, the attitude of women teachers about breast cancer and its screening methods is positive, but most do not refer to breast screening [16]. Ramli found a relationship between women’s health beliefs and mammography [17]. However, very few studies have been conducted on other factors related to screening tests for common cancers in Iran.
The Health Belief Model (HBM) has been widely used to assess health beliefs about cancer screening behaviors; it is a cognitive model that attempts to identify health behavior patterns. In general, this model focuses on changes in beliefs that lead to changes in behaviors [18, 19]. The effectiveness of this model has been reported on issues such as breast self-examination [20], breast cancer screening behavior [21], thalassemia education in high school students [22], and so on. In internal studies, it is affected on breast cancer screening behaviors [23], effect of education based on health belief model on the behavior of breast cancer screening [24]. Considering the rising trend of breast cancer in Iran, this study aimed to determine breast cancer screening behaviors based on HBM in Mashhad.
Materials and Methods
This study is an analytical cross-sectional study. The samples consisted of 406 women referred to five health centers in Mashhad City and agreed to participate in the study. The sample size was estimated based on previous studies. According to the previously published research, the actual frequency of perceived severity (one of the constructs of the health belief model) was 58% [25], and considering an attrition rate of 10%, the sample size is presented as it follows: (Z=1.96; P=0.58; d=0.05). The inclusion criteria were the ability to read, write, and speak in Persian, residence in Mashhad for at least 5 years, and no history of breast cancer. The exclusion criteria included people who completed the questionnaires incompletely or did not answer the questions at all. The study was carried out from July 2018 to May 2019, after the Ethics Committee approved the research project.
Based on the multistage cluster sampling method, each one of five major health centers in Mashhad was considered one cluster (five clusters in total). Besides, there was also a list of other health centers they covered. Then, each cluster was divided into subcategories based on the socioeconomic similarities of the districts. Next, one district was randomly selected from each cluster, and two health centers were randomly chosen from the list of centers in that region. The subjects with the inclusion criteria were selected from the patients of these centers. They were selected by the convenience sampling method.
The data collection tool was a questionnaire consisting of two parts. The first part collected sociodemographic data, including age, marital status, education, occupation, spouse occupation, household income, number of family members, insurance status, and family history of breast cancer. The second part consisted of questions based on Health Belief Model (HBM) constructs that measure women’s beliefs about breast cancer screening. This part contains 83 items that were answered based on a 5-point Likert scale. Each item has 5 response choices ranging from strong disagreement (1 point) to strong agreement (5 points). The HBM constracts were the perceived susceptibility (3 items, the score range: 3 to 15), perceived severity (12 items, the score range: 12 to 60), perceived benefits (16 items, the score range: 16 to 80), perceived barriers (25 items, the score range: 25 to 125), cues to action (6 items, the score range: 6 to 30), and self-efficacy (18 items, the score range: 18 to 90) [26]. In this study, the psychometric version in Persian of this tool has been used [27].
The researcher attends the selected health centers after receiving the research approval from the University Ethics Committee and obtaining a referral letter from Mashhad School of Nursing and Midwifery. Then, the researcher submitted the referral letter to the authorities of the five health centers of Mashhad. After obtaining the women’s consent to participate in the research, they were given an informed consent form, and the data were completed by face-to-face interview.
The data were analyzed in SPSS software, v. 16. To describe the data, statistical indices, standard deviation, and frequency distribution tables were used. Also, we used the Kolmogorov- Smirnov to check the normal distribution of data and the Pearson and Spearman tests for data analyses.
Results
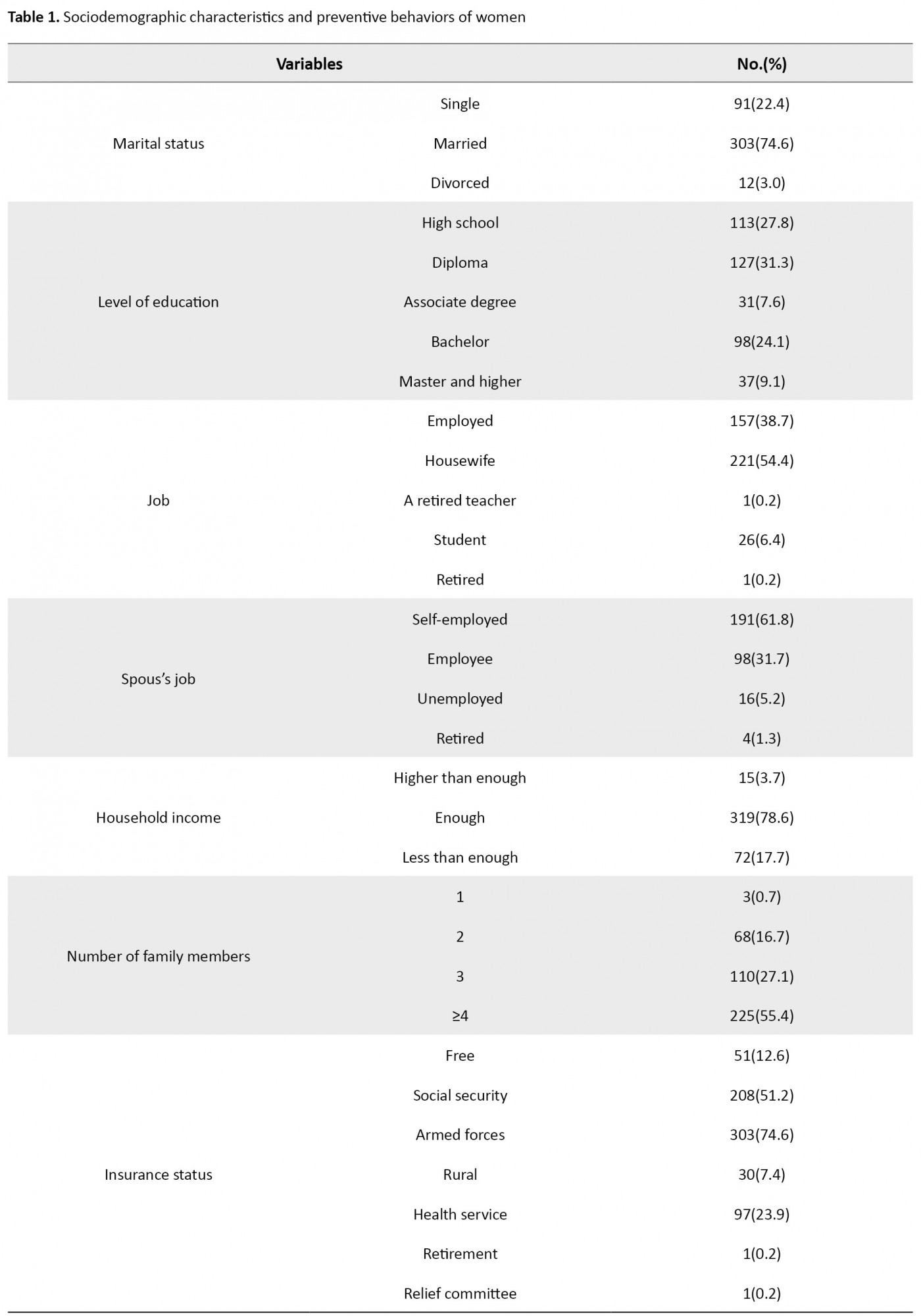
In this study, 406 women were studied. The Mean±SD age of the women was 33.5±10.3 years. Table 1 presents the sociodemographic characteristics and breast screening behaviors of the women under study.
.jpg)
To determine the normal distribution of data, we used the Kolmogorov-Smirnov test. The Mean±SD score of health belief model constructs related to cancer screening behavior in women were as follows: perceived susceptibility, 66.4±18.9; perceived severity, 50.1±21.4; perceived benefits, 28.8±16.6; perceived barriers, 59.0±16.4; cues to action, 38.3±18.7; and self-efficacy 56.2±17.5.
Table 2 presents the severity of health belief model constructs among women about cancer screening behavior.
.jpg)
One percent of women had very low susceptibility. The self-efficacy of 2.2% of women was very low.
Table 3 presents the correlation between health belief models constructs.
.jpg)
The results of the Pearson correlation coefficient showed that the relationship between perceived barriers and perceived benefits was negative and significant (P=0.001, r=-0.160) (Table 3).
Regarding the relationship between health belief constructs and women’s preventive behaviors, the Spearman statistical test did not show significant relationships between preventive behavior with perceived susceptibility, perceived severity, perceived benefits, and perceived barriers. But this test showed significant relationships between preventive behavior with self-efficacy (P=0.001, r=0.896) and cues to action (P=0.001, r=0.269) (Table 4).
.jpg)
The Pearson correlation test did not show significant relationships between self-efficacy and education, job, spouse’s job, and income. However, this test showed a negative and significant statistical relationship between age and self-efficacy (P=0.001, r=-0.231).
Discussion
This study examines breast cancer screening behaviors in women in Mashhad health centers and determines its relationship with the constructs of the health belief model. Considering the results, the breast screening behaviors of women were undesirable. Most women did not have a clinical breast exam. Almost half of them did not do breast self-examinations during the last year. Many women did not refer for physician’s examination during the last year and mammography in the last three years. Women in the Amani et al. study had a better performance concerning mammography and breast self-examination [28]. This difference may be related to education, occupation, and the context of conducting research. Women in the Zahedi’s study performed better than women in the present study in performing breast self-examination, clinical breast examination by a physician, and mammography [29].
The results showed that the women had moderate to high susceptibility and perceived severity of breast cancer screening behaviors. They also had good self-efficacy but did not understand the benefits of breast screening and felt many barriers to breast cancer screening, too. Considering the results, women in the present study perceived fewer benefits for performing breast cancer prevention behaviors. But lack of knowledge or awareness of the benefits of breast cancer screening was not related to women’s performance. The factor that led the women to study breast cancer screening was not its perceived benefits but the women’s sense of self-efficacy. The results of this study are in line with the Sahraeiʼs study results. She reported that only 10.9% of women have regular breast self-examinations, and self-efficacy was a strong predictor of breast self-examination [30].
Considering the results, perceived benefits are directly related to perceived severity. The higher the perceived severity of the disease outcomes, the greater a person’s belief in positive outcomes associated with breast cancer prevention behaviors. Different perceived barriers within various levels (individual, intrapersonal, health systems, and community) play influential roles in women’s decisions to participate in breast cancer screening program. Another area where women are less likely to be screened for breast cancer is perceived barriers to their understanding. In summary, different barriers influence women’s decisions to undergo breast cancer screening behaviors. In the present study, most women reported moderate and high perceived barriers to breast screening. In another study, the most important perceived barriers to breast screening were lack of awareness, barriers to access (financial, geographical, cultural), fear (of consequences and pain), the performance of service providers, women’s beliefs, delaying screening, embarrassment, long wait for receiving care [31].
The results demonstrated that perceived barriers had a statistically significant relationship with perceived susceptibility and perceived severity but are inversely related to perceived benefits. The cue to action is directly related to perceived benefits. Perceived severity has a significant relationship with perceived susceptibility. Perceived benefits are directly related to perceived severity. But only self-efficacy and cues to action could predict breast cancer screening behaviors. HBM recognizes that sometimes wanting to change a health behavior is not enough to make someone do it. Accordingly, two more elements are necessary to get an individual to leap. In other words, two elements of cues to action and self-efficacy predict cancer screening behavior. Self-efficacy has statistically significant relationships with perceived susceptibility, cue to action, and perceived benefits.
Self-efficacy looks at people’s beliefs in their abilities to make health-related changes. If women believe that they are at risk and know potential positive aspects of changing behavior to reduce the threat of disease, they have greater confidence in their ability and thus are more likely to engage in healthy behaviors. In Momenyan et al. [32], Hosseini et al. [33], and Teymouri and Habibi [34] studies, there was a significant relationship between self-efficacy and breast self-examination. The results of the present study are consistent with their results. To explain this relationship, it can be said that women that feel and believe in more self-efficacy to prevent or control breast cancer are more engaged in breast cancer screening behaviors. A person with self-efficacy feels empowered in doing a particular activity, adopts health-promoting behaviors, and quits harmful behavior. Therefore, understanding self-efficacy can help maintain health-promoting behaviors. People with low self-efficacy have a more challenging time looking at issues and will have a one-dimensional, superficial view of problems. Self-efficacy means the belief in oneself to perform a particular behavior successfully and expect the results. Self-efficacy is an essential prerequisite for behavior. Self-efficacy affects a person’s motivation and forces the person to strive and persevere in behavior [35].
Other results in the self-efficacy section showed that the sense of self-efficacy decreases with age. In the study of Teymouri and Habibi, the sense of self-efficacy reduced with the increasing age of women [34]. One of the reasons for these findings is that as women get older, they feel that they can no longer take care of themselves or recognize the symptoms of the disease in their bodies earlier. Studies have shown that self-efficacy varies with age. In both sexes, self-efficacy increases throughout childhood and early adulthood, peaks in middle age, and decreases after age 60 [36].
The present study results showed that although the women in the study felt moderate to high self-efficacy, but did not show good performance in this area. A small percentage of women underwent clinical breast examination by a physician last year or have been referred for mammography for the past three years. The present study results are consistent with the results of Hosseini’s study [33]. These results suggest that women think they have a lower chance of developing breast cancer. The studies have mentioned another reason for not performing screening behaviors, which was related to not feeling problems and pain in the breast. Women avoid screening behaviors because they think that they should have a breast self-examination or visit by a doctor only if they have abnormal signs and symptoms in their breasts. This misconception is a major reason for many women who do not perform screening behavior [36].
A cue to action is something that helps move someone from wanting to make a health change to actually making the change. They are external events that prompt a desire to make a change. Cues in the environment trigger action and act on individual perceptions, such as perceived benefits. The present study results are similar to the results of Masoudi’s study [37].
The health belief model is based on the theory that individuals’ tendency to change toward healthier behaviors depends on factors, such as perceived susceptibility, perceived severity, perceived benefits, and perceived barriers. Therefore, it can recognize the concerns of women for breast cancer screening behaviors. This study showed that breast self-examination behaviors (self-examination, clinical examination, and mammography) in women are low and undesirable. Self-efficacy and cues to action are the two main components of the HBM in performing breast cancer screening behaviors. Self-efficacy, which actually reflects a person’s perception of performing the appropriate behavior to achieve the desired condition, has been introduced in many studies as a predictor of health behaviors, including self-examination and clinical breast examination. Therefore, by strengthening self-efficacy through educational programs, women can adopt appropriate behavior. Limitations of the present study included uncontrolled factors such as the subject’s personality, cultural models, the effects of social class on behavior, and level of expectation which can influence the answers to questionnaires.
Since self-efficacy in the present study has been found to be the main factor for performing breast cancer prevention behaviors, it is suggested to examine the factors that increase self-efficacy to perform screening behaviors in women of different reproductive ages.
Ethical Considerations
Compliance with ethical guidelines
The study participants were informed about the study objectives, and they and one of their parents signed an informed consent form. They were also assured of the confidentiality of their information. Moreover, they were allowed to leave the study, and the study results would be available to them. This study obtained its ethical approval (IR. MUMS. REC. 2016. 593) from Mashhad University of Medical Sciences.
Funding
This research was supported by Mashhad University of Medical Sciences.
Authors' contributions
Study concept and design, manuscript preparation: Morvarid Irani, Fatemeh Ghaffari Sardasht, and Khadije Mizaii Najmabadi; Literature review and statistical analysis: Maryam Fasanghari, Fatemeh Ghaffari, and Morvarid Irani; Designing, reviewing the questionnaire and manuscript review: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The research team would like to thank the directors of the health centers from where participants were recruited for their cooperation and easing the data collection process.
References
In 2020, 2.3 million women were diagnosed with breast cancer, and 685000 of them died globally. As of the end of 2020, there were 7.8 million women alive who have been diagnosed with breast cancer in the past 5 years, making it the world’s most prevalent cancer. There are more lost disability-adjusted life years by women due to breast cancer globally than any other type of cancer [1]. According to an estimate in 2020, the greatest cancer-related mortality will be observed in developing countries. In contrast, disease burden will reduce in Western countries due to the healthy lifestyle and better health facilities [2]. In Iran, breast cancer has been identified as the most common cancer and the fifth leading cause of death among Iranian women. The standardized incidence rate is about 28 per 100000 people, which has increased in recent years [3].
Every year, millions of cancer patients could be saved from premature death and suffering if they had timely access to early detection and treatment [4]. Survival for breast cancer is generally good, particularly if it is diagnosed early [5]. The most effective early detection methods are breast self-examination, mammography, and clinical breast examinations by physicians and healthcare professionals [6]. Breast cancer mortality is reduced by 40% in women aged 40-74 years who participate in screening every 1-2 years [7]. Breast self-examination can help detect 10% of breast cancer cases, especially in younger women who did not undergo mammography [8]. Secondary prevention through monthly breast self-examination is the best option to tackle the rising incidence of breast cancer [9]. A study has shown that age, level of education, information about breast cancer, family history of cancer, and understanding the importance of screening are influential factors in performing breast cancer self-examination [10]. Another breast cancer screening method is the clinical breast examination by a physician. About two-thirds of the reduction in breast cancer mortality could be attributed to clinical breast examination [11].
In the study of Tuyen, 15.8% of women underwent clinical breast examination [12]. Mammography is one of the best screening methods. This method is an early and timely diagnosis of breast cancer before it reaches a diameter of 5 mm [13]. Use of mammography in women under 50 with timely diagnosis and treatment of cancer results in a 5-year relative survival rate of around 90% [14]. According to the investigations, despite the availability of appropriate, accessible, and low-cost screening programs for all individuals, public acceptance of using these facilities is negligible [15]. In the Alharbi study, the attitude of women teachers about breast cancer and its screening methods is positive, but most do not refer to breast screening [16]. Ramli found a relationship between women’s health beliefs and mammography [17]. However, very few studies have been conducted on other factors related to screening tests for common cancers in Iran.
The Health Belief Model (HBM) has been widely used to assess health beliefs about cancer screening behaviors; it is a cognitive model that attempts to identify health behavior patterns. In general, this model focuses on changes in beliefs that lead to changes in behaviors [18, 19]. The effectiveness of this model has been reported on issues such as breast self-examination [20], breast cancer screening behavior [21], thalassemia education in high school students [22], and so on. In internal studies, it is affected on breast cancer screening behaviors [23], effect of education based on health belief model on the behavior of breast cancer screening [24]. Considering the rising trend of breast cancer in Iran, this study aimed to determine breast cancer screening behaviors based on HBM in Mashhad.
Materials and Methods
This study is an analytical cross-sectional study. The samples consisted of 406 women referred to five health centers in Mashhad City and agreed to participate in the study. The sample size was estimated based on previous studies. According to the previously published research, the actual frequency of perceived severity (one of the constructs of the health belief model) was 58% [25], and considering an attrition rate of 10%, the sample size is presented as it follows: (Z=1.96; P=0.58; d=0.05). The inclusion criteria were the ability to read, write, and speak in Persian, residence in Mashhad for at least 5 years, and no history of breast cancer. The exclusion criteria included people who completed the questionnaires incompletely or did not answer the questions at all. The study was carried out from July 2018 to May 2019, after the Ethics Committee approved the research project.
Based on the multistage cluster sampling method, each one of five major health centers in Mashhad was considered one cluster (five clusters in total). Besides, there was also a list of other health centers they covered. Then, each cluster was divided into subcategories based on the socioeconomic similarities of the districts. Next, one district was randomly selected from each cluster, and two health centers were randomly chosen from the list of centers in that region. The subjects with the inclusion criteria were selected from the patients of these centers. They were selected by the convenience sampling method.
The data collection tool was a questionnaire consisting of two parts. The first part collected sociodemographic data, including age, marital status, education, occupation, spouse occupation, household income, number of family members, insurance status, and family history of breast cancer. The second part consisted of questions based on Health Belief Model (HBM) constructs that measure women’s beliefs about breast cancer screening. This part contains 83 items that were answered based on a 5-point Likert scale. Each item has 5 response choices ranging from strong disagreement (1 point) to strong agreement (5 points). The HBM constracts were the perceived susceptibility (3 items, the score range: 3 to 15), perceived severity (12 items, the score range: 12 to 60), perceived benefits (16 items, the score range: 16 to 80), perceived barriers (25 items, the score range: 25 to 125), cues to action (6 items, the score range: 6 to 30), and self-efficacy (18 items, the score range: 18 to 90) [26]. In this study, the psychometric version in Persian of this tool has been used [27].
The researcher attends the selected health centers after receiving the research approval from the University Ethics Committee and obtaining a referral letter from Mashhad School of Nursing and Midwifery. Then, the researcher submitted the referral letter to the authorities of the five health centers of Mashhad. After obtaining the women’s consent to participate in the research, they were given an informed consent form, and the data were completed by face-to-face interview.
The data were analyzed in SPSS software, v. 16. To describe the data, statistical indices, standard deviation, and frequency distribution tables were used. Also, we used the Kolmogorov- Smirnov to check the normal distribution of data and the Pearson and Spearman tests for data analyses.
Results
In this study, 406 women were studied. The Mean±SD age of the women was 33.5±10.3 years. Table 1 presents the sociodemographic characteristics and breast screening behaviors of the women under study.
.jpg)
To determine the normal distribution of data, we used the Kolmogorov-Smirnov test. The Mean±SD score of health belief model constructs related to cancer screening behavior in women were as follows: perceived susceptibility, 66.4±18.9; perceived severity, 50.1±21.4; perceived benefits, 28.8±16.6; perceived barriers, 59.0±16.4; cues to action, 38.3±18.7; and self-efficacy 56.2±17.5.
Table 2 presents the severity of health belief model constructs among women about cancer screening behavior.
.jpg)
One percent of women had very low susceptibility. The self-efficacy of 2.2% of women was very low.
Table 3 presents the correlation between health belief models constructs.
.jpg)
The results of the Pearson correlation coefficient showed that the relationship between perceived barriers and perceived benefits was negative and significant (P=0.001, r=-0.160) (Table 3).
Regarding the relationship between health belief constructs and women’s preventive behaviors, the Spearman statistical test did not show significant relationships between preventive behavior with perceived susceptibility, perceived severity, perceived benefits, and perceived barriers. But this test showed significant relationships between preventive behavior with self-efficacy (P=0.001, r=0.896) and cues to action (P=0.001, r=0.269) (Table 4).
.jpg)
The Pearson correlation test did not show significant relationships between self-efficacy and education, job, spouse’s job, and income. However, this test showed a negative and significant statistical relationship between age and self-efficacy (P=0.001, r=-0.231).
Discussion
This study examines breast cancer screening behaviors in women in Mashhad health centers and determines its relationship with the constructs of the health belief model. Considering the results, the breast screening behaviors of women were undesirable. Most women did not have a clinical breast exam. Almost half of them did not do breast self-examinations during the last year. Many women did not refer for physician’s examination during the last year and mammography in the last three years. Women in the Amani et al. study had a better performance concerning mammography and breast self-examination [28]. This difference may be related to education, occupation, and the context of conducting research. Women in the Zahedi’s study performed better than women in the present study in performing breast self-examination, clinical breast examination by a physician, and mammography [29].
The results showed that the women had moderate to high susceptibility and perceived severity of breast cancer screening behaviors. They also had good self-efficacy but did not understand the benefits of breast screening and felt many barriers to breast cancer screening, too. Considering the results, women in the present study perceived fewer benefits for performing breast cancer prevention behaviors. But lack of knowledge or awareness of the benefits of breast cancer screening was not related to women’s performance. The factor that led the women to study breast cancer screening was not its perceived benefits but the women’s sense of self-efficacy. The results of this study are in line with the Sahraeiʼs study results. She reported that only 10.9% of women have regular breast self-examinations, and self-efficacy was a strong predictor of breast self-examination [30].
Considering the results, perceived benefits are directly related to perceived severity. The higher the perceived severity of the disease outcomes, the greater a person’s belief in positive outcomes associated with breast cancer prevention behaviors. Different perceived barriers within various levels (individual, intrapersonal, health systems, and community) play influential roles in women’s decisions to participate in breast cancer screening program. Another area where women are less likely to be screened for breast cancer is perceived barriers to their understanding. In summary, different barriers influence women’s decisions to undergo breast cancer screening behaviors. In the present study, most women reported moderate and high perceived barriers to breast screening. In another study, the most important perceived barriers to breast screening were lack of awareness, barriers to access (financial, geographical, cultural), fear (of consequences and pain), the performance of service providers, women’s beliefs, delaying screening, embarrassment, long wait for receiving care [31].
The results demonstrated that perceived barriers had a statistically significant relationship with perceived susceptibility and perceived severity but are inversely related to perceived benefits. The cue to action is directly related to perceived benefits. Perceived severity has a significant relationship with perceived susceptibility. Perceived benefits are directly related to perceived severity. But only self-efficacy and cues to action could predict breast cancer screening behaviors. HBM recognizes that sometimes wanting to change a health behavior is not enough to make someone do it. Accordingly, two more elements are necessary to get an individual to leap. In other words, two elements of cues to action and self-efficacy predict cancer screening behavior. Self-efficacy has statistically significant relationships with perceived susceptibility, cue to action, and perceived benefits.
Self-efficacy looks at people’s beliefs in their abilities to make health-related changes. If women believe that they are at risk and know potential positive aspects of changing behavior to reduce the threat of disease, they have greater confidence in their ability and thus are more likely to engage in healthy behaviors. In Momenyan et al. [32], Hosseini et al. [33], and Teymouri and Habibi [34] studies, there was a significant relationship between self-efficacy and breast self-examination. The results of the present study are consistent with their results. To explain this relationship, it can be said that women that feel and believe in more self-efficacy to prevent or control breast cancer are more engaged in breast cancer screening behaviors. A person with self-efficacy feels empowered in doing a particular activity, adopts health-promoting behaviors, and quits harmful behavior. Therefore, understanding self-efficacy can help maintain health-promoting behaviors. People with low self-efficacy have a more challenging time looking at issues and will have a one-dimensional, superficial view of problems. Self-efficacy means the belief in oneself to perform a particular behavior successfully and expect the results. Self-efficacy is an essential prerequisite for behavior. Self-efficacy affects a person’s motivation and forces the person to strive and persevere in behavior [35].
Other results in the self-efficacy section showed that the sense of self-efficacy decreases with age. In the study of Teymouri and Habibi, the sense of self-efficacy reduced with the increasing age of women [34]. One of the reasons for these findings is that as women get older, they feel that they can no longer take care of themselves or recognize the symptoms of the disease in their bodies earlier. Studies have shown that self-efficacy varies with age. In both sexes, self-efficacy increases throughout childhood and early adulthood, peaks in middle age, and decreases after age 60 [36].
The present study results showed that although the women in the study felt moderate to high self-efficacy, but did not show good performance in this area. A small percentage of women underwent clinical breast examination by a physician last year or have been referred for mammography for the past three years. The present study results are consistent with the results of Hosseini’s study [33]. These results suggest that women think they have a lower chance of developing breast cancer. The studies have mentioned another reason for not performing screening behaviors, which was related to not feeling problems and pain in the breast. Women avoid screening behaviors because they think that they should have a breast self-examination or visit by a doctor only if they have abnormal signs and symptoms in their breasts. This misconception is a major reason for many women who do not perform screening behavior [36].
A cue to action is something that helps move someone from wanting to make a health change to actually making the change. They are external events that prompt a desire to make a change. Cues in the environment trigger action and act on individual perceptions, such as perceived benefits. The present study results are similar to the results of Masoudi’s study [37].
The health belief model is based on the theory that individuals’ tendency to change toward healthier behaviors depends on factors, such as perceived susceptibility, perceived severity, perceived benefits, and perceived barriers. Therefore, it can recognize the concerns of women for breast cancer screening behaviors. This study showed that breast self-examination behaviors (self-examination, clinical examination, and mammography) in women are low and undesirable. Self-efficacy and cues to action are the two main components of the HBM in performing breast cancer screening behaviors. Self-efficacy, which actually reflects a person’s perception of performing the appropriate behavior to achieve the desired condition, has been introduced in many studies as a predictor of health behaviors, including self-examination and clinical breast examination. Therefore, by strengthening self-efficacy through educational programs, women can adopt appropriate behavior. Limitations of the present study included uncontrolled factors such as the subject’s personality, cultural models, the effects of social class on behavior, and level of expectation which can influence the answers to questionnaires.
Since self-efficacy in the present study has been found to be the main factor for performing breast cancer prevention behaviors, it is suggested to examine the factors that increase self-efficacy to perform screening behaviors in women of different reproductive ages.
Ethical Considerations
Compliance with ethical guidelines
The study participants were informed about the study objectives, and they and one of their parents signed an informed consent form. They were also assured of the confidentiality of their information. Moreover, they were allowed to leave the study, and the study results would be available to them. This study obtained its ethical approval (IR. MUMS. REC. 2016. 593) from Mashhad University of Medical Sciences.
Funding
This research was supported by Mashhad University of Medical Sciences.
Authors' contributions
Study concept and design, manuscript preparation: Morvarid Irani, Fatemeh Ghaffari Sardasht, and Khadije Mizaii Najmabadi; Literature review and statistical analysis: Maryam Fasanghari, Fatemeh Ghaffari, and Morvarid Irani; Designing, reviewing the questionnaire and manuscript review: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The research team would like to thank the directors of the health centers from where participants were recruited for their cooperation and easing the data collection process.
References
- World Health Organization (WHO). Cancer fact sheets: Breast cancer [Internet]. 2021 [Updated 2021 March 26]. Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer
- Mubarik S, Malik SS, Wang Z, Li C, Fawad M, Yu C. Recent insights into breast cancer incidence trends among four Asian countries using age-period-cohort model. Cancer Management and Research. 2019; 11:8145-55. [DOI:10.2147/CMAR.S208323] [PMID] [PMCID]
- Shamshirian A, Heydari K, Shams Z, Aref AR, Shamshirian D, Tamtaji OR, et al. Breast cancer risk factors in Iran: A systematic review & meta-analysis. Hormone Molecular Biology and Clinical Investigation. 2020; 41(4). [DOI:10.1515/hmbci-2020-0021] [PMID]
- Toporcov TN, Wünsch Filho V. Epidemiological science and cancer control. Clinics. 2018; 73(suppl 1):e627s. [DOI:10.6061/clinics/2018/e627s] [PMID] [PMCID]
- Rivera-Franco MM, Leon-Rodriguez E. Delays in breast cancer detection and treatment in developing countries. Breast Cancer: Basic and Clinical Research. 2018; 12:1178223417752677. [DOI:10.1177/1178223417752677] [PMID] [PMCID]
- Mohammadifard M, Khazaee Z, Mohammadifard M. [The needs for screening of breast cancer, based on the latest guidelines (Persian)]. Journal of Birjand University of Medical Sciences. 2019; 26(1):1-3. [DOI:10.32592/JBirjandUnivMedSci.2019.26.1.100]
- Seely JM, Alhassan T. Screening for breast cancer in 2018-what should we be doing today? Current Oncology. 2018; 25(Suppl 1):S115-24. [DOI:10.3747/co.25.3770] [PMID] [PMCID]
- Salim KS, Al-Attar WMA, Alani BG. Breast self- examination practice among female students in Iraq. Systematic Reviews in Pharmacy. 2021; 12(2):516-20. https://www.sysrevpharm.org/abstract/-examination-practice-among-female-students-in-iraq-67296.html
- Dagne AH, Ayele AD, Assefa EM. Assessment of breast self-examination practice and associated factors among female workers in Debre Tabor Town public health facilities, North West Ethiopia, 2018: Cross-sectional study. PloS One. 2019; 14(8):e0221356. [DOI:10.1371/journal.pone.0221356] [PMID] [PMCID]
- Tazhibi M, Feizi A. Awareness levels about breast cancer risk factors, early warning signs, and screening and therapeutic approaches among Iranian adult women: A large population based study using latent class analysis. BioMed Research International. 2014; 2014:306352. [DOI:10.1155/2014/306352] [PMID] [PMCID]
- Mittra I, Mishra GA, Dikshit RP, Gupta S, Kulkarni VY, Shaikh HK, et al. Effect of screening by clinical breast examination on breast cancer incidence and mortality after 20 years: Prospective, cluster randomised controlled trial in Mumbai. British Medical Journal. 2021; 372:n256. [DOI:10.1136/bmj.n256] [PMID] [PMCID]
- Tuyen DQ, Dung TV, Dong HV, Kien TT, Huong TT. Breast self-examination: knowledge and practice among female textile workers in Vietnam. Cancer Control. 2019; 26(1):1073274819862788. [DOI:10.1177/1073274819862788] [PMID] [PMCID]
- Moghaddam Tabrizi F, Vahdati S, Khanahmadi S, Barjasteh S. Determinants of breast cancer screening by mammography in women referred to health centers of Urmia, Iran. Asian Pacific Journal of Cancer Prevention. 2018; 19(4):997-1003. [DOI:10.22034/APJCP.2018.19.4.997] [PMID] [PMCID]
- Morris E, Feig SA, Drexler M, Lehman C. Implications of overdiagnosis: Impact on screening mammography practices. Population Health Management. 2015; 18(Suppl 1):S3-S11. [DOI:10.1089/pop.2015.29023.mor] [PMID] [PMCID]
- da Costa Vieira RA, Biller G, Uemura G, Ruiz CA, Curado MP. Breast cancer screening in developing countries. Clinics. 2017; 72(4):244-53. [DOI:10.6061/clinics/2017(04)09] [PMID] [PMCID]
- Alharbi NA, Alshammari MS, Almutairi BM, Makboul G, El-Shazly MK. Knowledge, awareness, and practices concerning breast cancer among Kuwaiti female school teachers. Alexandria Journal of Medicine. 2012; 48(1):75-82. [DOI:10.1016/j.ajme.2011.10.003]
- Ramli HA, Moey SF, Mutalib AM. The relationship of health beliefs on the stage of mammography behavior adoption amongst women in Kuantan, Pahang. Asian Pacific Journal of Cancer Prevention. 2019; 20(6):1913-20. [DOI:10.31557/APJCP.2019.20.6.1913] [PMID] [PMCID]
- Namdar A, Bigizadeh Sh, Naghizadeh MM. [Behaviors preventive adopting in components model belief health measuring cancer cervical towards (Persian)]. Journal of Fasa University of Medical Sciences. 2012; 2(1):34-44. [DOR:20.1001.1.22285105.2012.2.1.7.1]
- Khodaveisi M, Salehi Khah M, Bashirian S, Karami M, Khodaveisi M. The effect of health belief model-based training on preventive behaviors of hepatitis b in addicts. International Journal of High Risk Behaviors and Addiction. 2018; 7(2):e58579. [DOI:10.5812/ijhrba.58579]
- Norman P, Brain K. An application of the health belief model to the prediction of breast selfexamination in a national sample of women with a family history of breast cancer. British Journal of Health Psychology. 2005; 10(Pt 1):1-16. [DOI:10.1348/135910704X24752] [PMID]
- VanDyke SD, Shell MD. Health beliefs and breast cancer screening in rural Appalachia: An evaluation of the health belief model. The Journal of Rural Health. 2017; 33(4):350-60. [DOI:10.1111/jrh.12204] [PMID]
- Masoudi GR, Rezaie Kykha R, Shahraki Poor M, Naderi M, Zareban I. The effect of halth belief model-based training on preventing major thalassemia in thalassemia carrier couples. Journal of Research and Health. 2015; 5(2):211-9. http://jrh.gmu.ac.ir/article-1-164-en.html
- Darvishpour A, Vajari SM, Noroozi S. Can health belief model predict breast cancer screening behaviors? Open Access Macedonian Journal of Medical Sciences. 2018; 6(5):949-53. [DOI:10.3889/oamjms.2018.183] [PMID] [PMCID]
- Masoudi Yekta L, Rezaei-Bayatiyani H, Dashtbozorgi B, Gheibizadeh M, Malehi AS, Moradi M. Effect of education based on health belief model on the behavior of breast cancer screening in women. Asia-Pacific Journal of Oncology Nursing. 2018; 5(1):114-20. [DOI:10.4103/apjon.apjon_36_17] [PMID] [PMCID]
- Khazir Z, Sharifabad MA, Vaezi AA, Enjezab B, Fallahzadeh H, Yari F. Predictors of mammography based on Health Belief Model in Khorramabad women. Journal of Education and Health Promotion. 2019; 8:180. [DOI:10.4103/jehp.jehp_63_19] [PMID] [PMCID]
- Champion V, Skinner CS, Menon U. Development of a self-efficacy scale for mammography. Research in Nursing & Health. 2005; 28(4):329-36. [DOI:10.1002/nur.20088] [PMID]
- Taymoori P, Berry T. The validity and reliability of champion’s health belief model scale for breast cancer screening behaviors among Iranian women. Cancer Nursing. 2009; 32(6):465-72. [DOI:10.1097/NCC.0b013e3181aaf124] [PMID]
- Amani M, Mirhaghjou SN, Niknami M, Kazem Nezhad Leyli E. The status of screening tests for women’s common cancers in the personnel of the educational-medical and health centers. Journal of Holistic Nursing and Midwifery. 2018; 28(4):246-51. [DOI:10.29252/hnmj.28.4.246]
- Zahedi R, Rezapour M, Molavi Vardanjani H, Baneshi MR, Haghdoost AA, Malekpour Afshar R, et al. Breast cancer risk perception and screening behaviors of Iranian Women. Women’s Health Bulletin. 2021; 24(2):63-71. [DOI:10.30476/WHB.2021.89925.1103]
- Sahraei A, Noroozi A, Tahmasebi R. [Predicting factors of breast self-examination based on health belief model and locus of control among women aged 20-50 years (Persian)]. Hayat. 2013; 19(2):27-39. http://hayat.tums.ac.ir/article-1-1145-en.html
- Azami-Aghdash S, Ghojazadeh M, Sheyklo SG, Daemi A, Kolahdouzan K, Mohseni M, et al. Breast cancer screening barriers from the womans perspective: A meta-synthesis. Asian Pacific Journal of Cancer Prevention. 2015; 16(8):3463-71. [DOI:10.7314/APJCP.2015.16.8.3463] [PMID]
- Momenyan S, Rangraz Jedi M, Sanei Irani F, Adibi Garakhani Z, Sarvi F. [Prediction of breast self-examination in a sample of nursing and midwifery students Qom city using health belief model, Iran (Persian)]. Qom University of Medical Sciences Journal. 2014; 8(2):28-33. http://journal.muq.ac.ir/article-1-174-en.html
- Hoseini ZS, Mohaddes Hakak H, Lashkardoost H, Khankolabi M, Mehri A, Salari E. Effect of awareness and perceived self-efficacy on breast cancer preventive behaviors in women: A case study of Neyshabur City. Journal of Education Community Health. 2019; 6(1):33-9. [DOI:10.29252/jech.6.1.33]
- Taymoori P, Habibi S. [Application of a health belief model for explaining mammography behavior by using structural equation model in women in Sanandaj (Persian)]. Scientific Journal of Kurdistan University of Medical Sciences. 2014; 19(3):103-15. [DOI:10.22102/19.3.12]
- Abdolkarimy M, Zareipour M, Mahmoodi H, Dashti S, Faryabi R, Movahed E. [Health promoting behaviors and their relationship with self-efficacy of health workers (Persian)]. Iran Journal of Nursing. 2017; 30(105):68-79. [DOI:10.29252/ijn.30.105.68]
- Naseh L, Shaikhy R, Rafiei H. General self-efficacy and associated factors among elderly residents of nursing home. Journal of Holistic Nursing and Midwifery. 2016; 26(2):90-7. http://hnmj.gums.ac.ir/article-1-691-en.html
- Masoudi Yekta L, Dashtbozorgi B, Gheibizadeh M, Saki Malehi A, Moradi M. Applying the health belief model in predicting breast cancer screening behavior of women. Jundishapur Journal of Chronic Disease Care. 2015; 4(4):e30234. [DOI:10.17795/jjcdc-30234]
Article Type : Research |
Subject:
Special
Received: 2020/11/19 | Accepted: 2022/01/1 | Published: 2022/04/1
Received: 2020/11/19 | Accepted: 2022/01/1 | Published: 2022/04/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |