Sun, May 19, 2024
Volume 32, Issue 1 (1-2022)
JHNM 2022, 32(1): 69-77 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Tugbamenekli T, Yildirim Y. Complementary and Integrative Medicines Used by Cancer Patients to Cope With Chemotherapy-Related Taste Alterations. JHNM 2022; 32 (1) :69-77
URL: http://hnmj.gums.ac.ir/article-1-1795-en.html
URL: http://hnmj.gums.ac.ir/article-1-1795-en.html
1- Assistant Professor, Department of Internal Medicine Nursing, Faculty of Health Sciences, Malatya Turgut Özal University, Malatya, Turkey. , tugbamenekli2013@gmail.com
2- Professor, Department of Internal Medicine Nursing, Faculty of Nursing, Ege University, Izmir, Turkey.
2- Professor, Department of Internal Medicine Nursing, Faculty of Nursing, Ege University, Izmir, Turkey.
Full-Text [PDF 527 kb]
(442 Downloads)
| Abstract (HTML) (1150 Views)
Full-Text: (426 Views)
Introduction
Cancer is a group of diseases characterized by the uncontrolled proliferation of cells in any part of the body and has numerous signs, symptoms, and treatment approaches [1, 2, 3]. Cancer is also a life-threatening disease. The number of cancer patients has increased dramatically in recent decades. The morbidity and mortality of cancer were reported at a high level, and its cost and duration of treatment and adverse effects on the quality of life make it an emerging health crisis [4, 5, 6]. Cancer mortality increased about 20% from 1995 to 2018, and its cost in Europe was € 199 billion [7].
Today, one of the most common cancer treatments is chemotherapy. Chemotherapy affects not only cancer cells but also normal cells that causes numerous side effects [2, 6, 7]. Among these side effects, a change in the sense of taste frequently occurs. It was reported that between 38.8% and 86% of patients under chemotherapy experience taste alterations [8, 9]. Patients describe the change in the sense of taste as a metallic, bitter, or bad taste in their mouths, sensitivity or insensitivity to sweet tastes, and intolerance of bitter tastes [8, 10].
Taste is an important sense for the people, and there are five basic taste perceptions: sweet, sour, salty, bitter, and umami [10]. Chemotherapy affects the taste buds, which are responsible for the sense of taste and the secretion of saliva, and also has neurotoxic effects which lead to taste alterations [11, 12]. Taste alterations can affect food preferences, eating habits, and appetite, resulting in inadequate nutrition [5, 7]. This condition causes weight loss and adversely affects the energy intake to carry out daily activities. As a result, the shortage of nutrients and energy adversely affects the quality of life, social interactions, and disease prognosis [6, 10, 13].
In reducing or eliminating taste alterations that develop as a result of chemotherapy, patients can use Complementary and Integrative Medicine (CIM) methods instead of or along with pharmacological treatments [8, 10, 11, 14, 15]. Complementary medicine is a group of treatment methods aimed at supporting modern medicine, improving patients’ quality of life, reducing symptoms or the side effects of drugs, and providing physical and psychological support [1, 8, 16]. In the United States, according to NCCIH (the National Center for Complementary and Integrative Health), “integrative health brings conventional and complementary approaches together in a coordinated way” [9, 14, 15]. According to the World Health Organization (WHO), treatment approaches other than modern medicine are defined as complementary medicine [17]. Studies have shown that while complementary treatments may be beneficial in alleviating symptoms, plant products, in particular, can interact with chemotherapy drugs and cause various complications [9, 16]. Nurses should ask about and assess the use of CIM methods when a patient applies to a health care facility [15, 18]. The use of CIM methods recommended by unreliable sources of knowledge may not be suitable for the patients and may reduce the effectiveness of their cancer treatment [8, 12]. Nurses, as part of the holistic approach, have an essential role in detecting and preventing such drugs and CIM interactions. Concepts about the complementary health approaches have moved forward recently in line with the philosophy of holistic nursing, and guidelines have been prepared based on complementary and holistic nursing for clinical use [18, 19]. Thus, it is crucial to provide a qualified service of holistic nursing for nurses caring for cancer patients. They should enquire about the CIM methods used by patients to treat the change in the sense of taste. The patients must be advised to continue using proven methods and be prevented the use of methods that may be harmful [15, 19, 20].
However, there is a gap in the literature regarding the frequency of CIM use to cope with taste alterations among cancer patients. Thus, this study aimed to evaluate CIM used by cancer patients to cope with chemotherapy-related taste alterations and affecting factors.
The research questions were as follows:
• What is the frequency of using complementary and integrative treatment methods by cancer patients who experience taste alteration following chemotherapy?
• What are the complementary and integrative treatment methods used by cancer patients who experience taste alteration following chemotherapy?
Materials and Methods
The study has a cross-sectional design. The study population consisted of the patients undergoing chemotherapy treatment at İnönü University Malatya Turgut Özal Medical Center, Oncology Hospital, Malatya City, Turkey, from July to December 2020. The minimum number of the sample was calculated by G power as 318, considering a 95% confidence interval, α=0.05, based on an estimated effect size of 0.3 (small effect) and degree of freedom of 5. The research was carried out on 318 patients who agreed to participate in the study.
Patients who were at least 18 years old, had a cancer diagnosis for six months or more, received chemotherapy for at least three months, and experienced taste alteration for six months or more were enrolled in the study. The patients who did not experience any taste alteration were not included in the study.
The data collection form has two parts. The first part concerned the patient’s demographic data, and the second part was about the use of CIM. The data collection form was developed by the researchers in line with the literature [1, 9, 13, 15, 21]. This data collection consisted of questions about patients’ sociodemographic characteristics, disease-related characteristics, CIM use experiences, and attitudes towards CIM. The questions were about the patient (age, gender, marital status, income level, education level, occupation, and living place), about the illness (cancer type, family history of cancer, metastasis status, disease stage, and disease duration), and about the CIM (CIM information status, reasons for not using CIM, use of CIM for chemotherapy-related taste alterations, herbal treatments, purpose of using CIM, effect of its use, and source of information about CIM use). The questionnaire was given to patients diagnosed with cancer who had undergone chemotherapy for at least three months, whose sense of taste was affected, and were referred to the cancer center of the research environment.
The IBM program SPSS v. 25 was used for data analysis. In the statistical evaluation of the data, we used descriptive statistics (numbers, percentages, Means±SD, the Chi-square test, and the independent t-test. Multivariate logistic regression analysis was used to determine potential predictors of CIM use among patients. The statistically significant variables from the Chi-square test and t-test (age, duration of illness, female gender, living in a village, having a history of cancer in the family, having breast cancer, having information on CIM, using phytotherapy, having metastasis, and lacking complications) were included in regression analysis. P values less than 0.05 were considered statistically significant for all analyses.
Results
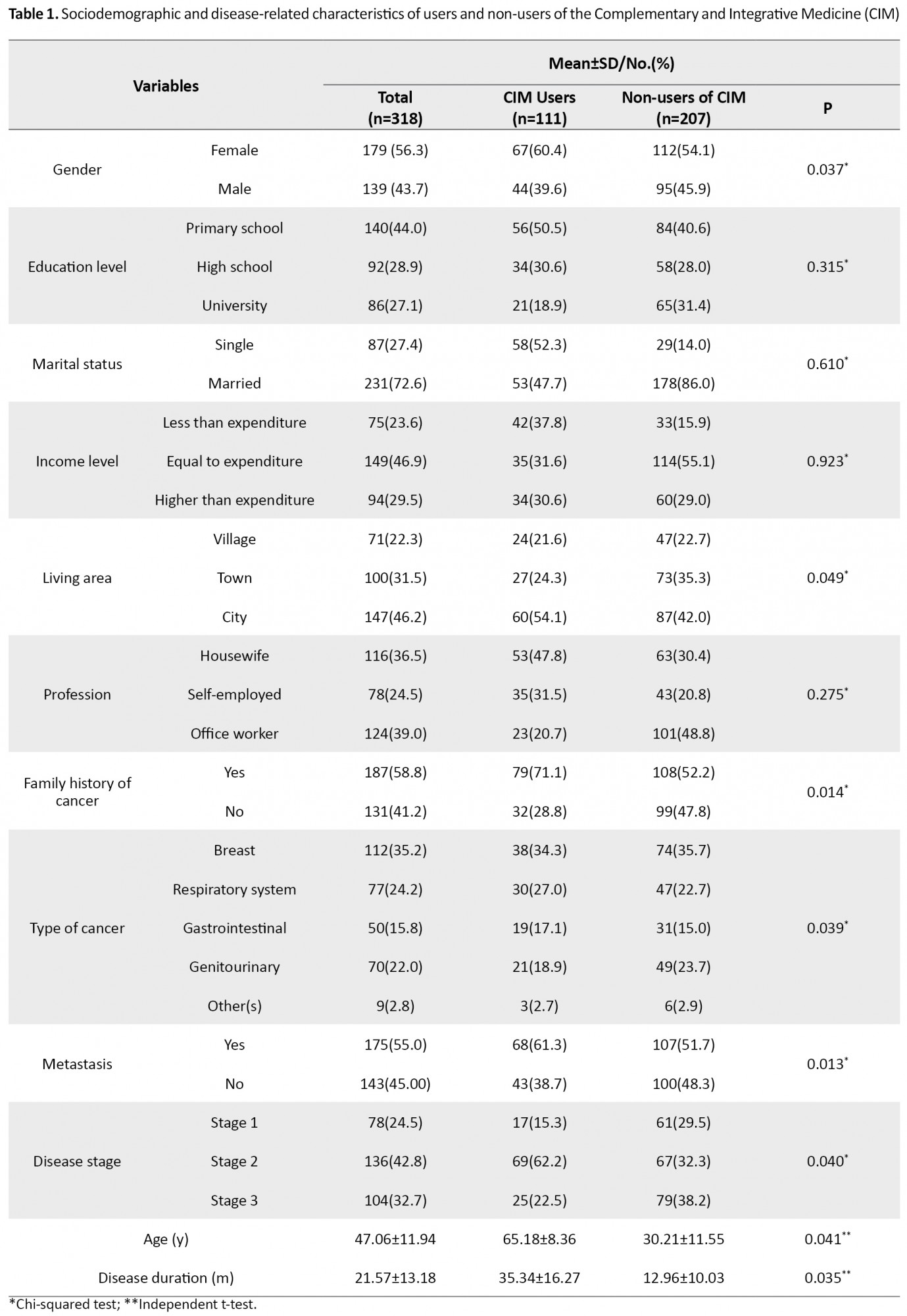
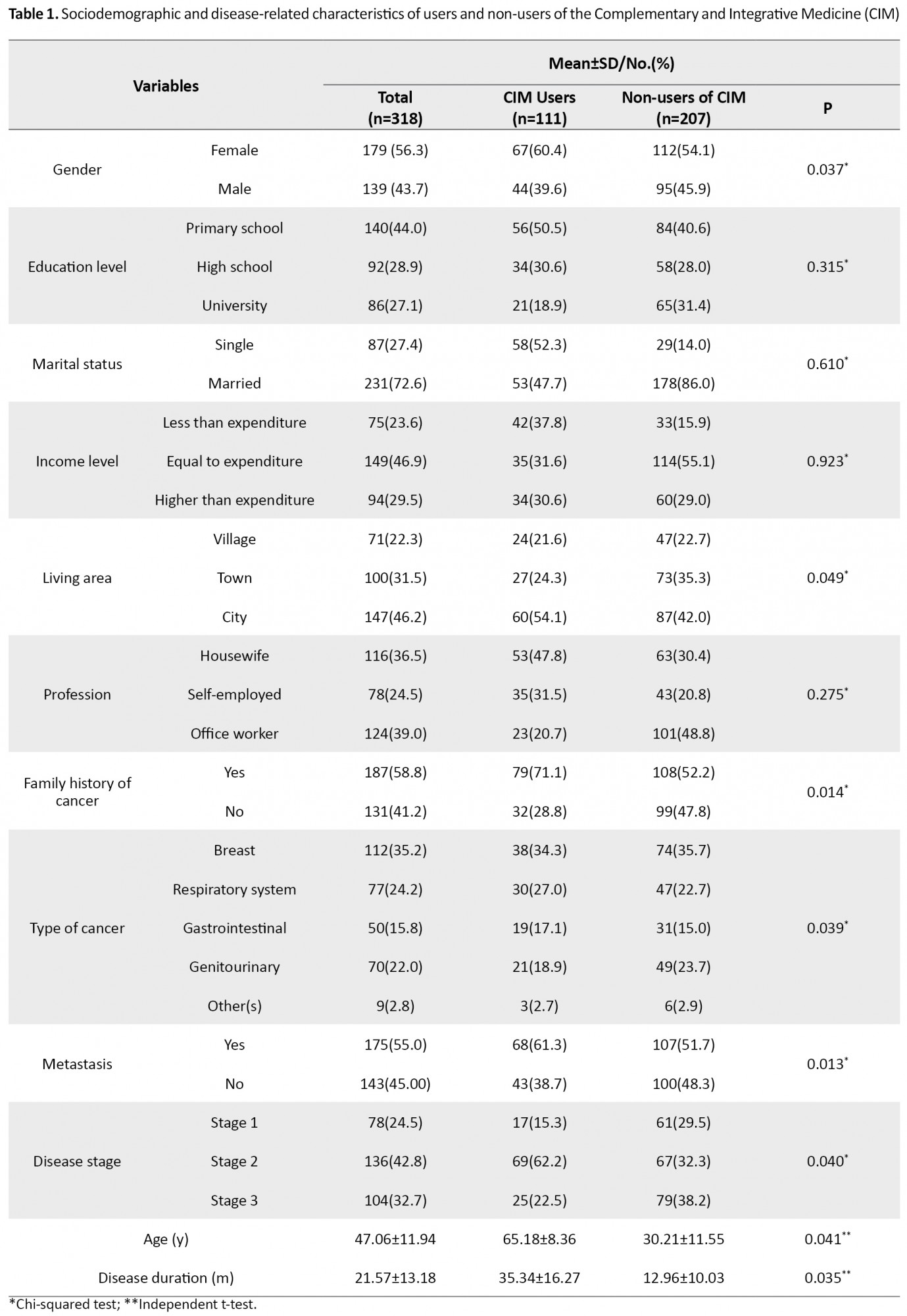
The Mean±SD age of the patients was 47.06±11.94 years, and the mean duration of their illness was 21.57±13.18 months. It was found that 34.9% of patients used at least one of the listed CIM modalities. There were significant differences between CIM users and non-users regarding age (P=0.041), gender (P=0.037), place of residence (P=0.049), having a history of cancer in the family (P=0.014), cancer type (P=0.039), metastasis (P=0.013), duration of illness (P=0.035), and stage of illness (P=0.040) (Table 1).
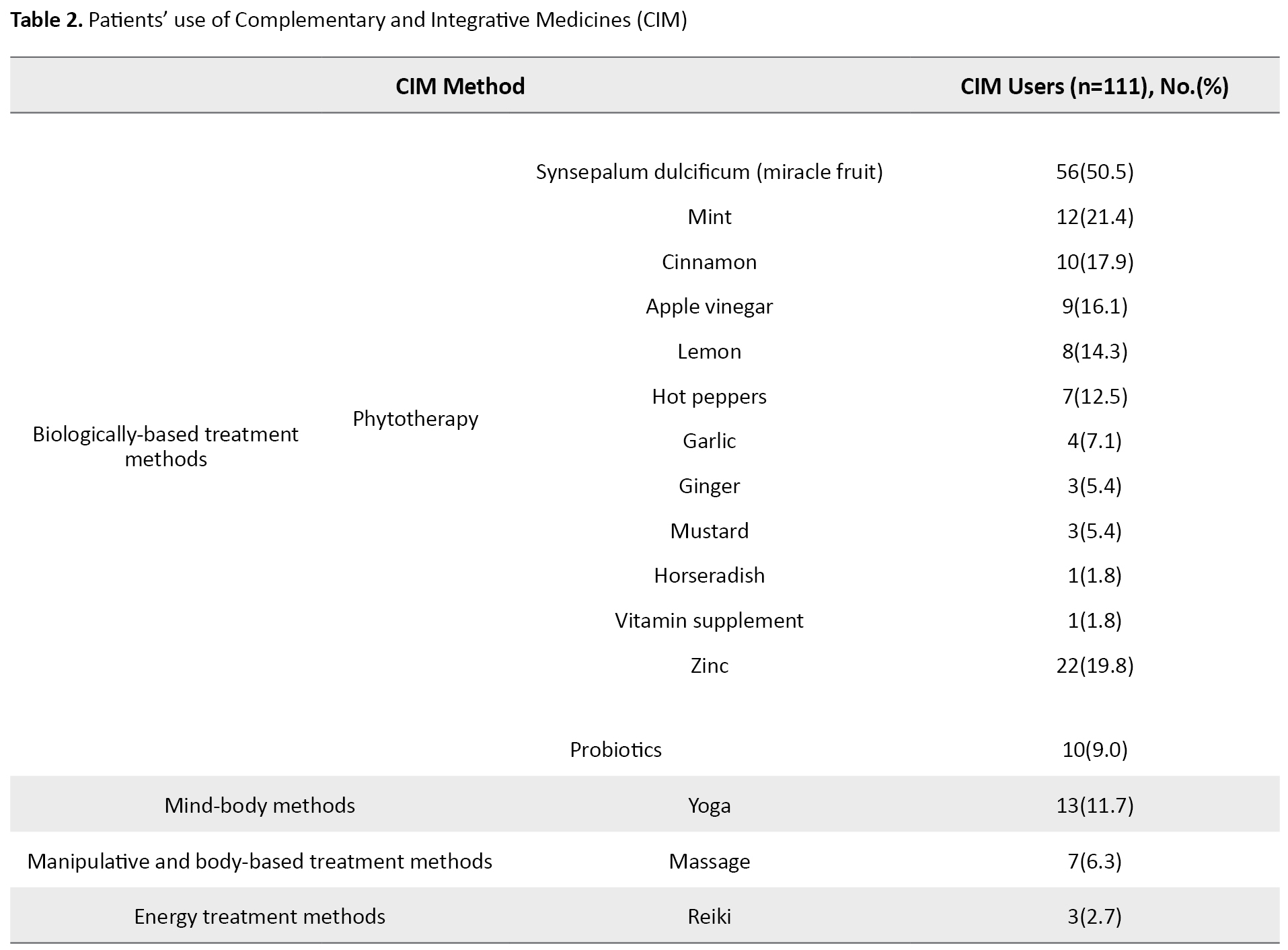
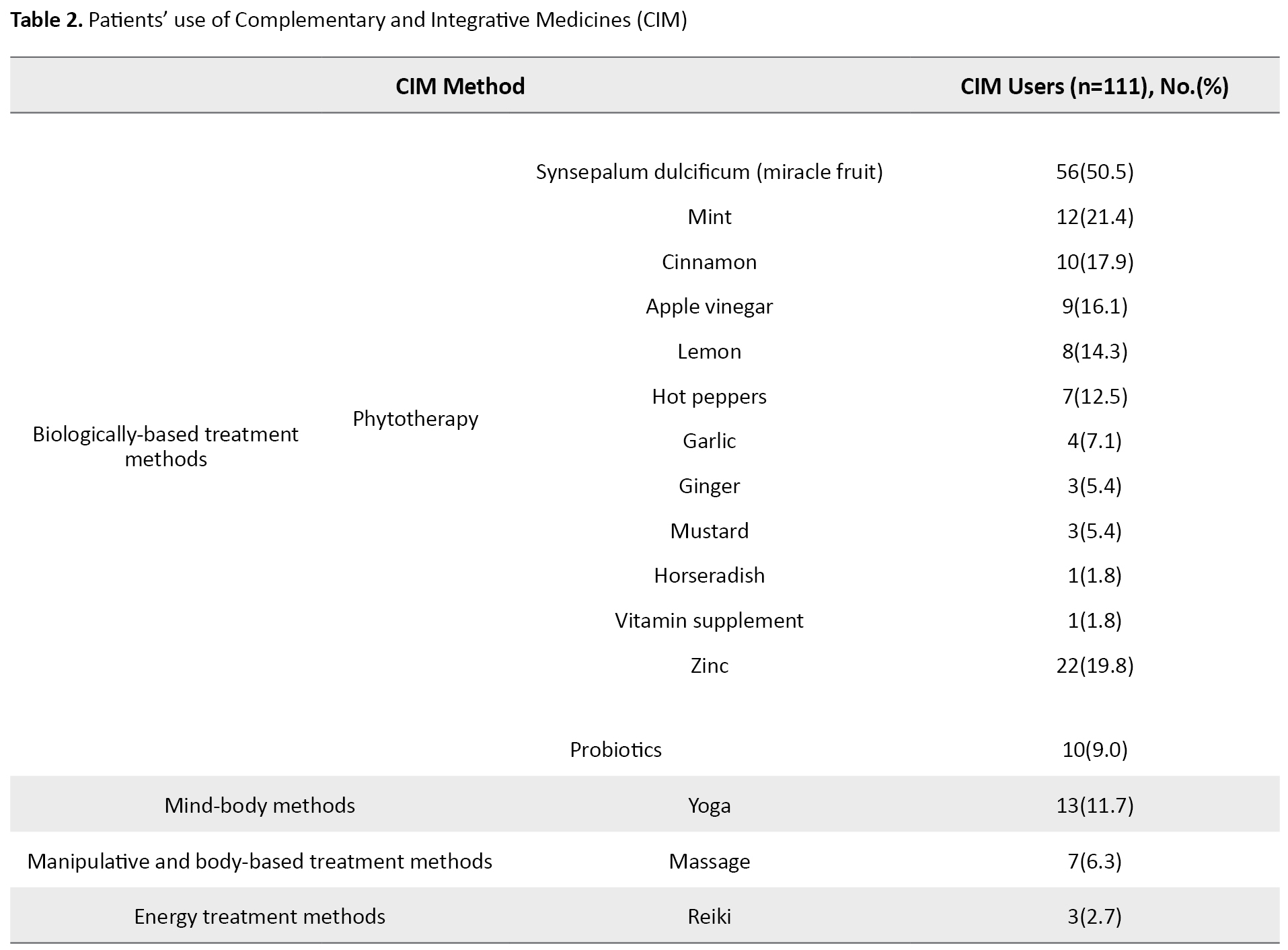
The most commonly-used CIM methods were phytotherapy (50.5%), zinc (19.8%), probiotics (9.0%), yoga (11.7%), massage (6.3%), and Reiki (2.7%) (Table 2).
It was found that 57.2% of the patients did not know about CIM methods, 55.6% did not use CIM methods because they thought it would be more hazardous, and 62.2% used CIM as an alternative method instead of the drugs used for taste alteration. We found that 76.6% of the patients felt better after using CIM, 94.6% did not experience complications when using CIM, and the source of 49.6% of the patients’ information about CIM was other patients. In addition, 83.8% of the patients recommended using CIM, 46.4% used the fruits for herbal treatment, and 62.5% consumed herbal medicines by boiling and drinking (Table 3).

The variables that show statistically significant difference between the CIM users and non-CIM users were evaluated by regression analysis (Table 4).

The factors increasing CIM use were lacking complications (B=0.903, 95%CI; 0.860-1.120, P=0.025), age (B=0.350, 95%CI; 0.120-0.475, P=0.032), duration of illness (B=0.175, 95% CI; 0.052-0.219, P=0.041), being female (B=0.244, 95%CI; 0.194-0.326, P=0.010), living in a city (B=0.035, 95%CI; 0.027-0.048, P=0.017), having a history of cancer in the family (B=0.324, 95%CI; 0.293-0.505, P=0.044), having a diagnosis of breast cancer (B=0.441, 95%CI; 0.305-0.737, P=0.026), having information about CIM (B= 0.017, 95% CI; 0.012-0.034, P=0.033), using phytotherapy (B=0.815, 95%CI; 0.678-0.944, P=0.018) and having metastasis (B=0.576, 95%CI; 0.423-0.781, P=0.030).
Discussion
A change in taste after chemotherapy is a frequent symptom among cancer patients. Despite the progress in managing symptoms in oncology, more than half of patients receiving chemotherapy are still suffering from taste alterations [10, 11, 22]. Thus, cancer patients frequently use CIM to cope with their symptoms [9, 20, 21].
We found that 34.9% of the patients used CIM to cope with taste alterations. As there are few studies in the literature examining CIM methods used to cope with taste alteration, the study results are compared with studies examining other symptoms in cancer patients, such as nausea, vomiting, mucositis, and diarrhea. In studies investigating the use of CIM by cancer patients in general, the frequencies of CIM use were reported between 26.0% and 51.0% [5, 12, 23]. The current study results are consistent with the literature on this topic. In recent years, the use of CIM has increased, especially in developing countries. It was reported that one-third of Americans use at least one CIM method in addition to the standard treatments [5, 12, 23].
In the current study, the three prevalent plants used were miracle fruit, mint, and cinnamon, in descending order. In studies examining the methods used by cancer patients to cope with their symptoms, it is emphasized that the most common method is phytotherapy [2, 5, 12, 18, 23]. It is believed that herbal products are natural and have no side effects; they can be used safely for a long time and alleviate symptoms. Also, they are cheap and readily available. However, it is also reported in the literature that various side effects may appear in connection with the form, dose, and duration of using herbal products. It is emphasized that more attention needs to be taken in CIM use, especially for cancer patients [20, 24]. Synsepalum dulcificum, known as miracle fruit, originates from West Africa, is used for chemotherapy-related taste alterations. The fruit contains a high amount of miraculin, a natural protein. It has an extraordinary ability to change taste stimuli in an acidic environment. It increases the pleasant taste of certain foods, reduces unpleasant tastes, and for a short time significantly changes the taste profiles of foods [25, 26, 27]. In a study evaluating the effects of miracle fruit in adult cancer patients under chemotherapy, it was reported that the sense of taste of all patients changed positively [28]. Also, it has been reported that the freshening effect of mint removes bitter tastes from the mouth, and cinnamon produces a sweet taste in the mouth [12, 23]. While methods such as homeopathy and relaxation treatments are used to manage symptoms such as pain, nausea, and vomiting in cancer patients, it was found that energy methods such as reflexology and mind-body approaches are rarely used for taste alterations [29, 30].
We found in the current study that the majority of CIM users employed these methods mainly as an alternative. In other studies, patients have stated that their reasons for using CIM are to reduce the symptoms of the illness, to prevent the recurrence of the disease, and to gain psychological relief. Also, they use CIM methods because they feel that these methods are beneficial. They believe CIM to be natural and safe and use it to overcome the illness and to feel physically and psychologically better [7, 23, 31, 32].
It was found that the patients’ primary source of information about CIM methods to cope with taste alterations are other patients, followed by advertisements and programs on the Internet and social media. Only a few participants have been advised by health professionals such as doctors, pharmacists, or nurses. It is reported in studies that the primary source of the information of CIM was the advice of other patients [32, 33]. This finding shows that the patients’ source of the CIM information is unreliable and based on personal experiences rather than scientific evidence. So the health professionals, especially nurses, should assess the patients’ CIM uses and their information on CIM [4, 34].
The predictive variables for CIM used to cope with taste alteration were, in the order of effectiveness, lacking complications, older age, duration of illness, being female, living in a city, having a history of cancer in the family, having a diagnosis of breast cancer, having knowledge of CIM, using phytotherapy, and having metastasis. Results that were sociodemographically similar to our own were obtained in various studies conducted on cancer patients in different places at different times [29, 30, 35]. This finding suggests that knowledge of CIM in patients and not experiencing complications will increase trust in the use of CIM and increase the frequency of use in patients. Older age increases the chronicity of illness and more symptoms, which may cause greater use of CIM to relieve these symptoms [6, 13]. Many women were housewives, and there are many health programs on daytime TV, and so it is thought that the women may have got information from these programs [8, 15].
Regarding the duration of illness, it was seen that after receiving a diagnosis, most patients put their trust in medical treatment. Still, over time they gave in to pessimism or a fear of death and began to seek other therapies [16, 18, 21]. Those with a breast cancer diagnosis used CIM more. This is because many patients taking part in the research were women. Patients living in cities were found to have a greater tendency to use CIM methods than patients living in small towns or villages. Some studies report greater resort to CIM methods by those living in villages than those living in cities [18, 33, 36]. However, the opposite result was achieved in our study. This finding indicates that CIM methods are not homogeneous in a country but vary region by region [12, 32]. When people living in a city receive a diagnosis, they may associate their illnesses with city pollution and stress. They mainly eat conventional agricultural products and have difficulty getting access to products containing fewer chemical fertilizers and pesticides—so-called organic products. These reasons may be connected to their desire to use CIM methods, which they see as natural and harmless [6, 29].
This study had some limitations. First, the study was conducted on participants diagnosed with cancer, but there was no comparison between particular cancer groups. Second, the participants were patients admitted to the hospital, and the study is not necessarily generalizable. Based on the study, we suggest that health professionals, especially nurses who frequently contact cancer patients, should be aware of high CIM use among patients. They also should examine the patient’s CIM use and the source of information on CIM. It is important to redirect patients to a reliable source of information on CIM. The CIM methods and their reliability should be included in nursing curricula and in-clinic training. Further studies are needed in larger groups and different populations.
Ethical Considerations
Compliance with ethical guidelines
Written permissions were obtained from the Medical Research Ethics Committee of the Turgut Özal University (Protocol: 20-6/15) and the hospital (Protocol: 8963064-120). Informed consent was read and signed by each participant. All principles of the Helsinki Declaration were followed throughout the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, methodology, investigation, writing - original, writing - review, and editing: Tugba Menekli; Data collection and data analysis: Tugba Menekli and Yasemin Yıldırım; Supervision: Yasemin Yıldırım.
Conflict of interest
The authors declared no conflict of interest.
References
Cancer is a group of diseases characterized by the uncontrolled proliferation of cells in any part of the body and has numerous signs, symptoms, and treatment approaches [1, 2, 3]. Cancer is also a life-threatening disease. The number of cancer patients has increased dramatically in recent decades. The morbidity and mortality of cancer were reported at a high level, and its cost and duration of treatment and adverse effects on the quality of life make it an emerging health crisis [4, 5, 6]. Cancer mortality increased about 20% from 1995 to 2018, and its cost in Europe was € 199 billion [7].
Today, one of the most common cancer treatments is chemotherapy. Chemotherapy affects not only cancer cells but also normal cells that causes numerous side effects [2, 6, 7]. Among these side effects, a change in the sense of taste frequently occurs. It was reported that between 38.8% and 86% of patients under chemotherapy experience taste alterations [8, 9]. Patients describe the change in the sense of taste as a metallic, bitter, or bad taste in their mouths, sensitivity or insensitivity to sweet tastes, and intolerance of bitter tastes [8, 10].
Taste is an important sense for the people, and there are five basic taste perceptions: sweet, sour, salty, bitter, and umami [10]. Chemotherapy affects the taste buds, which are responsible for the sense of taste and the secretion of saliva, and also has neurotoxic effects which lead to taste alterations [11, 12]. Taste alterations can affect food preferences, eating habits, and appetite, resulting in inadequate nutrition [5, 7]. This condition causes weight loss and adversely affects the energy intake to carry out daily activities. As a result, the shortage of nutrients and energy adversely affects the quality of life, social interactions, and disease prognosis [6, 10, 13].
In reducing or eliminating taste alterations that develop as a result of chemotherapy, patients can use Complementary and Integrative Medicine (CIM) methods instead of or along with pharmacological treatments [8, 10, 11, 14, 15]. Complementary medicine is a group of treatment methods aimed at supporting modern medicine, improving patients’ quality of life, reducing symptoms or the side effects of drugs, and providing physical and psychological support [1, 8, 16]. In the United States, according to NCCIH (the National Center for Complementary and Integrative Health), “integrative health brings conventional and complementary approaches together in a coordinated way” [9, 14, 15]. According to the World Health Organization (WHO), treatment approaches other than modern medicine are defined as complementary medicine [17]. Studies have shown that while complementary treatments may be beneficial in alleviating symptoms, plant products, in particular, can interact with chemotherapy drugs and cause various complications [9, 16]. Nurses should ask about and assess the use of CIM methods when a patient applies to a health care facility [15, 18]. The use of CIM methods recommended by unreliable sources of knowledge may not be suitable for the patients and may reduce the effectiveness of their cancer treatment [8, 12]. Nurses, as part of the holistic approach, have an essential role in detecting and preventing such drugs and CIM interactions. Concepts about the complementary health approaches have moved forward recently in line with the philosophy of holistic nursing, and guidelines have been prepared based on complementary and holistic nursing for clinical use [18, 19]. Thus, it is crucial to provide a qualified service of holistic nursing for nurses caring for cancer patients. They should enquire about the CIM methods used by patients to treat the change in the sense of taste. The patients must be advised to continue using proven methods and be prevented the use of methods that may be harmful [15, 19, 20].
However, there is a gap in the literature regarding the frequency of CIM use to cope with taste alterations among cancer patients. Thus, this study aimed to evaluate CIM used by cancer patients to cope with chemotherapy-related taste alterations and affecting factors.
The research questions were as follows:
• What is the frequency of using complementary and integrative treatment methods by cancer patients who experience taste alteration following chemotherapy?
• What are the complementary and integrative treatment methods used by cancer patients who experience taste alteration following chemotherapy?
Materials and Methods
The study has a cross-sectional design. The study population consisted of the patients undergoing chemotherapy treatment at İnönü University Malatya Turgut Özal Medical Center, Oncology Hospital, Malatya City, Turkey, from July to December 2020. The minimum number of the sample was calculated by G power as 318, considering a 95% confidence interval, α=0.05, based on an estimated effect size of 0.3 (small effect) and degree of freedom of 5. The research was carried out on 318 patients who agreed to participate in the study.
Patients who were at least 18 years old, had a cancer diagnosis for six months or more, received chemotherapy for at least three months, and experienced taste alteration for six months or more were enrolled in the study. The patients who did not experience any taste alteration were not included in the study.
The data collection form has two parts. The first part concerned the patient’s demographic data, and the second part was about the use of CIM. The data collection form was developed by the researchers in line with the literature [1, 9, 13, 15, 21]. This data collection consisted of questions about patients’ sociodemographic characteristics, disease-related characteristics, CIM use experiences, and attitudes towards CIM. The questions were about the patient (age, gender, marital status, income level, education level, occupation, and living place), about the illness (cancer type, family history of cancer, metastasis status, disease stage, and disease duration), and about the CIM (CIM information status, reasons for not using CIM, use of CIM for chemotherapy-related taste alterations, herbal treatments, purpose of using CIM, effect of its use, and source of information about CIM use). The questionnaire was given to patients diagnosed with cancer who had undergone chemotherapy for at least three months, whose sense of taste was affected, and were referred to the cancer center of the research environment.
The IBM program SPSS v. 25 was used for data analysis. In the statistical evaluation of the data, we used descriptive statistics (numbers, percentages, Means±SD, the Chi-square test, and the independent t-test. Multivariate logistic regression analysis was used to determine potential predictors of CIM use among patients. The statistically significant variables from the Chi-square test and t-test (age, duration of illness, female gender, living in a village, having a history of cancer in the family, having breast cancer, having information on CIM, using phytotherapy, having metastasis, and lacking complications) were included in regression analysis. P values less than 0.05 were considered statistically significant for all analyses.
Results
The Mean±SD age of the patients was 47.06±11.94 years, and the mean duration of their illness was 21.57±13.18 months. It was found that 34.9% of patients used at least one of the listed CIM modalities. There were significant differences between CIM users and non-users regarding age (P=0.041), gender (P=0.037), place of residence (P=0.049), having a history of cancer in the family (P=0.014), cancer type (P=0.039), metastasis (P=0.013), duration of illness (P=0.035), and stage of illness (P=0.040) (Table 1).
The most commonly-used CIM methods were phytotherapy (50.5%), zinc (19.8%), probiotics (9.0%), yoga (11.7%), massage (6.3%), and Reiki (2.7%) (Table 2).
It was found that 57.2% of the patients did not know about CIM methods, 55.6% did not use CIM methods because they thought it would be more hazardous, and 62.2% used CIM as an alternative method instead of the drugs used for taste alteration. We found that 76.6% of the patients felt better after using CIM, 94.6% did not experience complications when using CIM, and the source of 49.6% of the patients’ information about CIM was other patients. In addition, 83.8% of the patients recommended using CIM, 46.4% used the fruits for herbal treatment, and 62.5% consumed herbal medicines by boiling and drinking (Table 3).

The variables that show statistically significant difference between the CIM users and non-CIM users were evaluated by regression analysis (Table 4).

The factors increasing CIM use were lacking complications (B=0.903, 95%CI; 0.860-1.120, P=0.025), age (B=0.350, 95%CI; 0.120-0.475, P=0.032), duration of illness (B=0.175, 95% CI; 0.052-0.219, P=0.041), being female (B=0.244, 95%CI; 0.194-0.326, P=0.010), living in a city (B=0.035, 95%CI; 0.027-0.048, P=0.017), having a history of cancer in the family (B=0.324, 95%CI; 0.293-0.505, P=0.044), having a diagnosis of breast cancer (B=0.441, 95%CI; 0.305-0.737, P=0.026), having information about CIM (B= 0.017, 95% CI; 0.012-0.034, P=0.033), using phytotherapy (B=0.815, 95%CI; 0.678-0.944, P=0.018) and having metastasis (B=0.576, 95%CI; 0.423-0.781, P=0.030).
Discussion
A change in taste after chemotherapy is a frequent symptom among cancer patients. Despite the progress in managing symptoms in oncology, more than half of patients receiving chemotherapy are still suffering from taste alterations [10, 11, 22]. Thus, cancer patients frequently use CIM to cope with their symptoms [9, 20, 21].
We found that 34.9% of the patients used CIM to cope with taste alterations. As there are few studies in the literature examining CIM methods used to cope with taste alteration, the study results are compared with studies examining other symptoms in cancer patients, such as nausea, vomiting, mucositis, and diarrhea. In studies investigating the use of CIM by cancer patients in general, the frequencies of CIM use were reported between 26.0% and 51.0% [5, 12, 23]. The current study results are consistent with the literature on this topic. In recent years, the use of CIM has increased, especially in developing countries. It was reported that one-third of Americans use at least one CIM method in addition to the standard treatments [5, 12, 23].
In the current study, the three prevalent plants used were miracle fruit, mint, and cinnamon, in descending order. In studies examining the methods used by cancer patients to cope with their symptoms, it is emphasized that the most common method is phytotherapy [2, 5, 12, 18, 23]. It is believed that herbal products are natural and have no side effects; they can be used safely for a long time and alleviate symptoms. Also, they are cheap and readily available. However, it is also reported in the literature that various side effects may appear in connection with the form, dose, and duration of using herbal products. It is emphasized that more attention needs to be taken in CIM use, especially for cancer patients [20, 24]. Synsepalum dulcificum, known as miracle fruit, originates from West Africa, is used for chemotherapy-related taste alterations. The fruit contains a high amount of miraculin, a natural protein. It has an extraordinary ability to change taste stimuli in an acidic environment. It increases the pleasant taste of certain foods, reduces unpleasant tastes, and for a short time significantly changes the taste profiles of foods [25, 26, 27]. In a study evaluating the effects of miracle fruit in adult cancer patients under chemotherapy, it was reported that the sense of taste of all patients changed positively [28]. Also, it has been reported that the freshening effect of mint removes bitter tastes from the mouth, and cinnamon produces a sweet taste in the mouth [12, 23]. While methods such as homeopathy and relaxation treatments are used to manage symptoms such as pain, nausea, and vomiting in cancer patients, it was found that energy methods such as reflexology and mind-body approaches are rarely used for taste alterations [29, 30].
We found in the current study that the majority of CIM users employed these methods mainly as an alternative. In other studies, patients have stated that their reasons for using CIM are to reduce the symptoms of the illness, to prevent the recurrence of the disease, and to gain psychological relief. Also, they use CIM methods because they feel that these methods are beneficial. They believe CIM to be natural and safe and use it to overcome the illness and to feel physically and psychologically better [7, 23, 31, 32].
It was found that the patients’ primary source of information about CIM methods to cope with taste alterations are other patients, followed by advertisements and programs on the Internet and social media. Only a few participants have been advised by health professionals such as doctors, pharmacists, or nurses. It is reported in studies that the primary source of the information of CIM was the advice of other patients [32, 33]. This finding shows that the patients’ source of the CIM information is unreliable and based on personal experiences rather than scientific evidence. So the health professionals, especially nurses, should assess the patients’ CIM uses and their information on CIM [4, 34].
The predictive variables for CIM used to cope with taste alteration were, in the order of effectiveness, lacking complications, older age, duration of illness, being female, living in a city, having a history of cancer in the family, having a diagnosis of breast cancer, having knowledge of CIM, using phytotherapy, and having metastasis. Results that were sociodemographically similar to our own were obtained in various studies conducted on cancer patients in different places at different times [29, 30, 35]. This finding suggests that knowledge of CIM in patients and not experiencing complications will increase trust in the use of CIM and increase the frequency of use in patients. Older age increases the chronicity of illness and more symptoms, which may cause greater use of CIM to relieve these symptoms [6, 13]. Many women were housewives, and there are many health programs on daytime TV, and so it is thought that the women may have got information from these programs [8, 15].
Regarding the duration of illness, it was seen that after receiving a diagnosis, most patients put their trust in medical treatment. Still, over time they gave in to pessimism or a fear of death and began to seek other therapies [16, 18, 21]. Those with a breast cancer diagnosis used CIM more. This is because many patients taking part in the research were women. Patients living in cities were found to have a greater tendency to use CIM methods than patients living in small towns or villages. Some studies report greater resort to CIM methods by those living in villages than those living in cities [18, 33, 36]. However, the opposite result was achieved in our study. This finding indicates that CIM methods are not homogeneous in a country but vary region by region [12, 32]. When people living in a city receive a diagnosis, they may associate their illnesses with city pollution and stress. They mainly eat conventional agricultural products and have difficulty getting access to products containing fewer chemical fertilizers and pesticides—so-called organic products. These reasons may be connected to their desire to use CIM methods, which they see as natural and harmless [6, 29].
This study had some limitations. First, the study was conducted on participants diagnosed with cancer, but there was no comparison between particular cancer groups. Second, the participants were patients admitted to the hospital, and the study is not necessarily generalizable. Based on the study, we suggest that health professionals, especially nurses who frequently contact cancer patients, should be aware of high CIM use among patients. They also should examine the patient’s CIM use and the source of information on CIM. It is important to redirect patients to a reliable source of information on CIM. The CIM methods and their reliability should be included in nursing curricula and in-clinic training. Further studies are needed in larger groups and different populations.
Ethical Considerations
Compliance with ethical guidelines
Written permissions were obtained from the Medical Research Ethics Committee of the Turgut Özal University (Protocol: 20-6/15) and the hospital (Protocol: 8963064-120). Informed consent was read and signed by each participant. All principles of the Helsinki Declaration were followed throughout the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, methodology, investigation, writing - original, writing - review, and editing: Tugba Menekli; Data collection and data analysis: Tugba Menekli and Yasemin Yıldırım; Supervision: Yasemin Yıldırım.
Conflict of interest
The authors declared no conflict of interest.
References
- Alonzi S, Hoerger M, Perry LM, Chow LD, Manogue C, Cotogno P, et al. Changes in taste and smell of food during prostate cancer treatment. Supportive Care in Cancer. 2021; 29(6):2807-9. [DOI:10.1007/s00520-021-06050-x] [PMID]
- Liu G, Zong G, Doty RL, Sun Q. Prevalence and risk factors of taste and smell impairment in a nationwide representative sample of the US population: A cross-sectional study. BMJ Open. 2016; 6(11):e013246. [DOI:10.1136/bmjopen-2016-013246] [PMID] [PMCID]
- Spotten LE, Corish CA, Lorton CM, Ui Dhuibhir PM, O'Donoghue NC, O'Connor B, et al. Subjective and objective taste and smell changes in cancer. Annals of Oncology. 2017; 28(5):969-84. [DOI:10.1093/annonc/mdx018] [PMID]
- Keene MR, Heslop IM, Sabesan SS, Glass BD. Complementary and alternative medicine use in cancer: A systematic review. Complementary Therapies in Clinical Practice. 2019; 35:33-47. [DOI:10.1016/j.ctcp.2019.01.004] [PMID]
- Nagashekhara M, Murthy V, Mruthyunjaya AT, Li Ann L. An empirical study on traditional, complementary and alternative medicine usage among Malaysian cancer patients. Asian Pacific Journal of Cancer Prevention. 2015; 16(15):6237-41. [DOI:10.7314/APJCP.2015.16.15.6237] [PMID]
- Yildirim Y. Patterns of the use of complementary and alternative medicine in women with metastatic cancer. Cancer Nursing. 2010; 33(3):194-200. [DOI:10.1097/NCC.0b013e3181c295ac] [PMID]
- Drareni K, Dougkas A, Giboreau A, Laville M, Souquet PJ, Bensafi M. Relationship between food behavior and taste and smell alterations in cancer patients undergoing chemotherapy: A structured review. Seminars in Oncology. 2019; 46(2):160-72. [DOI:10.1053/j.seminoncol.2019.05.002] [PMID]
- Alvarez-Camacho M, Gonella S, Ghosh S, Kubrak C, Scrimger RA, Chu KP, et al. The impact of taste and smell alterations on quality of life in head and neck cancer patients. Quality of Life Research. 2016; 25(6):1495-504. [DOI:10.1007/s11136-015-1185-2] [PMID]
- Gonella S. [Taste disorders in cancer patients (Italian)]. Assistenza Infermieristica e Ricerca: AIR. 2013; 32(4):223-32. [PMID]
- Amézaga J, Alfaro B, Ríos Y, Larraioz A, Ugartemendia G, Urruticoechea A, et al. Assessing taste and smell alterations in cancer patients undergoing chemotherapy according to treatment. Supportive Care in Cancer. 2018; 26(12):4077-86. [DOI:10.1007/s00520-018-4277-z] [PMID]
- Boltong A, Keast R. The influence of chemotherapy on taste perception and food hedonics: A systematic review. Cancer Treatment Reviews. 2012; 38(2):152-63. [DOI:10.1016/j.ctrv.2011.04.008] [PMID]
- Paul M, Davey B, Senf B, Stoll C, Münstedt K, Mücke R, et al. Patients with advanced cancer and their usage of complementary and alternative medicine. Journal of Cancer Research and Clinical Oncology. 2013; 139(9):1515-22. [DOI:10.1007/s00432-013-1460-y] [PMID]
- de Vries YC, Boesveldt S, Kelfkens CS, Posthuma EE, van den Berg MMGA, de Kruif JTCM, et al. Taste and smell perception and quality of life during and after systemic therapy for breast cancer. Breast Cancer Research and Treatment. 2018; 170(1):27-34. [DOI:10.1007/s10549-018-4720-3] [PMID] [PMCID]
- Belqaid K, Tishelman C, Orrevall Y, Månsson-Brahme E, Bernhardson BM. Dealing with taste and smell alterations-A qualitative interview study of people treated for lung cancer. PloS One. 2018; 13(1):e0191117. [DOI:10.1371/journal.pone.0191117] [PMID] [PMCID]
- Boltong A, Aranda S, Keast R, Wynne R, Francis PA, Chirgwin J, et al. A prospective cohort study of the effects of adjuvant breast cancer chemotherapy on taste function, food liking, appetite and associated nutritional outcomes. PloS One. 2014; 9(7):e103512. [DOI:10.1371/journal.pone.0103512] [PMID] [PMCID]
- Sözeri E, Kutlutürkan S. Taste alteration in patients receiving chemotherapy. The Journal of Breast Health. 2015; 11(2):81-7. [PMID] [PMCID]
- World Health Organization (WHO). General guidelines for methodologies on research and evaluation of traditional medicine. Geneva: World Health Organization; 2000. https://apps.who.int/iris/handle/10665/66783
- Gok Metin Z, Izgu N, Karadas C, Arikan Donmez A. Perspectives of oncology nurses on complementary and alternative medicine in Turkey: A cross-sectional survey. Holistic Nursing Practice. 2018; 32(2):107-13. [DOI:10.1097/HNP.0000000000000256] [PMID]
- Ward Sullivan C, Leutwyler H, Dunn LB, Miaskowski C. A review of the literature on symptom clusters in studies that included oncology patients receiving primary or adjuvant chemotherapy. Journal of Clinical Nursing. 2018; 27(3-4):516-45. [DOI:10.1111/jocn.14057] [PMID] [PMCID]
- Epstein JB, Smutzer G, Doty RL. Understanding the impact of taste changes in oncology care. Supportive Care in Cancer. 2016; 24(4):1917-31. [DOI:10.1007/s00520-016-3083-8] [PMID]
- IJpma I, Renken RJ, Gietema JA, Slart RHJA, Mensink MGJ, Lefrandt JD, et al. Changes in taste and smell function, dietary intake, food preference, and body composition in testicular cancer patients treated with cisplatin-based chemotherapy. Clinical Nutrition. 2017; 36(6):1642-8. [DOI:10.1016/j.clnu.2016.10.013] [PMID]
- Altundag A, Cayonu M. Chemical senses in cancer patients. Current Pharmaceutical Design. 2016; 22(15):2264-9. [PMID]
- Koçaşlı S, Demircan Z. Herbal product use by the cancer patients in both the pre and post surgery periods and during chemotherapy. African Journal of Traditional, Complementary and Alternative Medicines. 2017; 14(2):325-33. [PMID] [PMCID]
- Gamper EM, Giesinger JM, Oberguggenberger A, Kemmler G, Wintner LM, Gattringer K, et al. Taste alterations in breast and gynaecological cancer patients receiving chemotherapy: Prevalence, course of severity, and quality of life correlates. Acta Oncologica. 2012; 51(4):490-6. [PMID]
- Gómez de Cedrón M, Wagner S, Reguero M, Menéndez-Rey A, de Molina AR. Miracle berry as a potential supplement in the control of metabolic risk factors in cancer. Antioxidants. 2020; 9(12):1282. [DOI:10.3390/antiox9121282] [PMID] [PMCID]
- Demesyeux L, Brym M, Valdes D, Collazo C, Chambers AH. Yield and miraculin content of nine miracle fruit (Synsepalum Dulcificum) morphotypes. Euphytica. 2020; 216(11):1-12. [DOI:10.1007/s10681-020-02710-x]
- Akinmoladun AC, Adetuyi AR, Komolafe K, Oguntibeju OO. Nutritional benefits, phytochemical constituents, ethnomedicinal uses and biological properties of Miracle fruit plant (Synsepalum dulcificum Shumach. & Thonn. Daniell). Heliyon. 2020; 6(12):e05837. [DOI:10.1016/j.heliyon.2020.e05837] [PMID] [PMCID]
- Wilken MK, Satiroff BA. Pilot study of” miracle fruit” to improve food palatability for patients receiving chemotherapy. Clinical Journal of Oncology Nursing. 2012; 16(5):E173-7. [DOI:10.1188/12.CJON.E173-E177] [PMID]
- Wode K, Henriksson R, Sharp L, Stoltenberg A, Hök Nordberg J. Cancer patients’ use of complementary and alternative medicine in Sweden: A cross-sectional study. BMC Complementary and Alternative Medicine. 2019; 19(1):62. [DOI:10.1186/s12906-019-2452-5] [PMID] [PMCID]
- Wortmann JK, Bremer A, Eich HT, Wortmann HP, Schuster A, Fühner J, et al. Use of complementary and alternative medicine by patients with cancer: A cross-sectional study at different points of cancer care. Medical Oncology. 2016; 33(7):78. [DOI:10.1007/s12032-016-0790-4] [PMID]
- Ponticelli E, Clari M, Frigerio S, De Clemente A, Bergese I, Scavino E, et al. Dysgeusia and health-related quality of life of cancer patients receiving chemotherapy: A cross-sectional study. European Journal of Cancer Care. 2017; 26(2):e12633. [DOI:10.1111/ecc.12633] [PMID]
- Singh KP, Kober KM, Dhruva AA, Flowers E, Paul SM, Hammer MJ, et al. Risk factors associated with chemotherapy-induced nausea in the week before the next cycle and impact of nausea on quality of life outcomes. Journal of Pain and Symptom Management. 2018; 56(3):352-62. [DOI:10.1016/j.jpainsymman.2018.05.019] [PMID]
- Irmak Z, Tanrıverdi Ö, Ödemiş H, Uysal DD. Use of complementary and alternative medicine and quality of life of cancer patients who received chemotherapy in Turkey. Complementary Therapies in Medicine. 2019; 44:143-50. [DOI:10.1016/j.ctim.2019.04.008] [PMID]
- Speck RM, DeMichele A, Farrar JT, Hennessy S, Mao JJ, Stineman MG, et al. Taste alteration in breast cancer patients treated with taxane chemotherapy: Experience, effect, and coping strategies. Supportive Care in Cancer. 2013; 21(2):549-55. [DOI:10.1007/s00520-012-1551-3] [PMID]
- Turcott JG, Juárez-Hernández E, De la Torre-Vallejo M, Sánchez-Lara K, Luvian-Morales J, Arrieta O. Value: Changes in the detection and recognition thresholds of three basic tastes in lung cancer patients receiving cisplatin and paclitaxel and its association with nutritional and quality of life parameters. Nutrition and Cancer. 2016; 68(2):241-9. [PMID]
- Toygar İ, Yeşilbalkan ÖU, Kürkütlü M, Temelli A. Complementary and alternative medicines used by cancer patients to cope with nausea. Health & Research Journal. 2020; 6(1):29-35. [DOI:10.12681/healthresj.23003]
Article Type : Research |
Subject:
General
Received: 2021/09/17 | Accepted: 2021/10/23 | Published: 2022/01/1
Received: 2021/09/17 | Accepted: 2021/10/23 | Published: 2022/01/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |