Thu, Apr 25, 2024
Volume 31, Issue 4 (9-2021)
JHNM 2021, 31(4): 219-226 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mossayebnezhad R, Niknami M, Pakseresht S, Kazemnezhad Leili E. Estimation of Fetal Weight by Clinical Methods and Ultrasonography and Comparing With Actual Birth Weight. JHNM 2021; 31 (4) :219-226
URL: http://hnmj.gums.ac.ir/article-1-1737-en.html
URL: http://hnmj.gums.ac.ir/article-1-1737-en.html
1- Instructor, Department of Midwifery, School of Nursing and Midwifery, Zanjan University of Medical Sciences, Zanjan, Iran.
2- Instructor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. , niknami@gums.ac.ir
3- Professor, Social Determinants of Health Research Center (SDHRC), Reproductive Health Research Center, Department of Obstetrics, Women Health Promotion, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Department of Biostatics, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
2- Instructor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. , niknami@gums.ac.ir
3- Professor, Social Determinants of Health Research Center (SDHRC), Reproductive Health Research Center, Department of Obstetrics, Women Health Promotion, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Department of Biostatics, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 918 kb]
(707 Downloads)
| Abstract (HTML) (1246 Views)
Full-Text: (1991 Views)
Introduction
Estimation of Fetal Weight (EFW) is an essential key in the decision-making process for obstetric planning and management [2, 1]. Assessment of fetal weight is an essential part of predicting fetal weight disorders that include intrauterine growth disorders (weight less than 10% relative to gestational age) and macrosomia (weight more than 90% relative to gestational age) [4, 3]. To prevent the fetal, neonatal, and maternal morbidities and mortalities associated with Intrauterine Growth Retardation (IUGR) and macrosomia neonates, accurate estimation of fetal weight is very important [5].
There are techniques for fetal weight estimation, most commonly, clinical and ultrasonography techniques. Clinical methods for fetal weight estimation include abdominal palpation, Johnson’s formula, and Insler’s formula (Dare’s) [8, 7, 6]. Johnson’s and Insler’s formulas are used uterine height measurement to estimate fetal weight. Measurement of uterine height is a standard clinical method in prenatal care that any midwife or health care provider can perform. So these formulas are recommended because they are simple, safe, low-cost, and acceptable methods for estimating fetal weight [9, 10].
Ultrasonography estimation of fetal weight is 20% more or less inconsistent with actual fetal weight, and this can lead to both false-positive and false-negative results in the third trimester of pregnancy [5, 11]. However, one study reported that all ultrasound formulas were highly accurate in fetal weight estimation, with only a 10% significant difference from the actual birth weight [12]. Another study reported the 100% sensitivity and 97.1% specificity of ultrasound in IUGR diagnosis, and its 48.1% sensitivity is, and 97.3% specificity in macrosomia diagnosis. Many researchers report that ultrasonography is as accurate as clinical methods in fetal weight estimation, and many studies say there are differences in this issue [13, 14, 15]; therefore, the role of clinical methods for EFW should be considered.
Another study reported that Insler’s formula is better in estimating fetal weight, while the results of another study showed that Johnson’s formula is more suitable [16]. In reports with a difference of ±500 g compared to the actual birth weight, the abdominal palpation’s sensitivity was 35.42%, Johnson’s formula 64.65%, Insler’s formula 67.68%. Also, the abdominal palpation’s specificity was 76%, Johnson’s formula 32.38%, and Insler’s formula 35.05%. When the difference was ±1000 g, the sensitivity of abdominal palpation was 20%, Johnson’s formula 50%, Insler’s formula 42.86%. Also, the abdominal palpation’s specificity was 94.33%, Johnson formula 52.03%, and Insler’s formula 54.73% [17, 18, 19].
Different methods are available for fetal weight estimation. A method with the lowest error and the highest accuracy is more suitable. So considering the importance of EFW and known complications of incorrect fetal weight estimation, the use of methods that are easy, inexpensive, and cost-effective is needed, especially in developing countries. Since delivery is not always done in the hospital, and many deliveries are done in deprived areas that do not have enough facilities, the importance of clinical methods becomes greater. Because of the cost of ultrasonography and its unavailability in many regions, it is essential to optimize diagnostic-treatment costs and present a suitable objective. This study was done to ensure the accuracy of clinical methods for EFW with Actual Birth Weight (ABW) in term pregnant women.
Materials and Methods
The present study is an assessment of the accuracy of diagnostic tests. The study was conducted from May to July 2018. According to a study of Haji Esmaeilou with a 95% confidence level, the Mean±SD weight was 1599/41 [20], and the acceptable amount of estimating error of 5%, we need 247 people. The methods used in this study were abdominal palpation, Johnson’s formula, Insler’s formula, and ultrasonography. The inclusion criteria included singleton pregnancy, gestational age of 37-41 weeks, and cephalic presentation. The exclusion criteria included the rupture of membranous, congenital malformation, and stillbirth.
Fetal weight by Insler’s formula was estimated by (weight in gr)=abdominal girth (cm) X symphysis fundal height (cm). Measurements are done by a tape measure of the Seca strip (German-made) with a precision of 1 mm. In measuring the height of the uterus, the distance between the upper extremity of the uterus and the upper edge of the symphysis of the pubis was considered to be zero points in the area of the symphysis of the pubis, and the strip meter stretched to the midline of the abdomen to the uterus and somewhere when the uterine peak was touched by the fingers; the height of the womb was measured in cm. To measure the abdominal circumference of the mother, the strip of the membrane in the position of the umbilicus passed through the abdomen and behind the mother, and the corresponding number was recorded in cm [6, 9, 10].
Fetal weight by Johnson’s formula was estimated by fetal weight (gr)=(symphysis fundal height - N)×155. In this formula, if the mother’s weight is over 90 kg, 1 cm of the height of the uterus is reduced. Also, for the calculation of N, the vaginal examination is performed: when the presenting part is at the minus station, N=13; presenting part was at ‘zero’ station, N=12; and presenting part was at plus station N=11. In measurements, the examination was done between contractions [6, 9].
The samples were followed up until delivery. The birth weight was measured by the Beurer digital scale (Germany) accurately 5 gr the first 24 hours of childbirth. The researcher carried a scale between the delivery room and the operating room when estimating the actual birth weight of the newborns. After obtaining written consent and recording the individual data, the weight and height of the mothers were measured. Then, in all clinical methods, after urination, the mother was placed in the supine position without knee bending. In this study, there was no limitation in delivery phases, both in the latent phase and in the active phase in the third trimester.
All clinical fetal weight measurements, including abdominal palpation, Johnson’s formula, Insler’s formula, were performed by a midwife (researcher) with at least two years of experience in obstetrics. The present study was conducted over three months. During this period, 700 pregnant women were referred to the therapeutic, educational center of the study environment, of which 400 were available, and among them, 247 pregnant women with inclusion criteria were examined.
All statistical analysis was performed in SPSS version 21. One-sample t-test, the Chi-square, and the Bland-Altman plot were used to compare the diagnostic value of fetal weight estimation methods. The difference between the fetal weight and the actual birth weight in all methods was considered significant when P <0.05 with the 1-sample test. For the error rate of methods with the difference was ±100 gr, the Chi-square test was used, and the accuracy of the studied methods was based on sensitivity and specificity in the classification of birth weights: below 2500 gr (low birth weight), 2500-4000 gr (normal birth weight) and above 4000 gr (high birth weight).
Results
The study results showed that the participating pregnant women had a Mean±SD age of 28.86±42.4 years (ranged 16-41 years), Mean±SD BMI of 32.98±6.0 kg/m2, and the Mean±SD gestational age of 39±1.04 weeks (ranged 37-41 weeks). The majority of women were multiparous (59.5%). The gender of the infant in the majority was male (52.6%), and the type of delivery in the majority was cesarean section (60.3%).
In the present study, the Mean±SD birth weight by clinical palpation was 3371.053±345.56 g, Mean±SD birth weight by Johnson’s was 3041.206±411.41 gr, Mean±SD birth weight with Insler’s was 3556.316±531.56) gr, Mean±SD birth weight by ultrasonography was 3294.28±380.0 gr, and Mean±SD actual birth weight was 3343.352±432.79) gr (Table 1).
.jpg)
One-sample t-test showed that abdominal palpation (P=0.261) and ultrasonography (P=0.118) were not significantly different with actual birth weight, but Johnson’s formula (P=0.001) and Insler’s formula (P=0.001) were significantly different with actual birth weight (Table 2).
.jpg)
In the group of the fetal weight of below 2500 gr, the Insler’s formula was more accurate in estimating fetal weight. In the normal weight range group, the highest accuracy belonged to Johnson’s formula, and at weights above 4000 gr, the abdominal palpation method was a better predictor in the estimation of fetal weight (Table 3).
.jpg)
In this study, the Bland-Altman plot indicated that the difference in fetal weight with actual birth weight in abdominal palpation and ultrasonography had no significant statistical difference, but there was a statistical difference with Johnson’s and Insler’s methods (Figures 1, 2, 3, 4).
Estimation of Fetal Weight (EFW) is an essential key in the decision-making process for obstetric planning and management [2, 1]. Assessment of fetal weight is an essential part of predicting fetal weight disorders that include intrauterine growth disorders (weight less than 10% relative to gestational age) and macrosomia (weight more than 90% relative to gestational age) [4, 3]. To prevent the fetal, neonatal, and maternal morbidities and mortalities associated with Intrauterine Growth Retardation (IUGR) and macrosomia neonates, accurate estimation of fetal weight is very important [5].
There are techniques for fetal weight estimation, most commonly, clinical and ultrasonography techniques. Clinical methods for fetal weight estimation include abdominal palpation, Johnson’s formula, and Insler’s formula (Dare’s) [8, 7, 6]. Johnson’s and Insler’s formulas are used uterine height measurement to estimate fetal weight. Measurement of uterine height is a standard clinical method in prenatal care that any midwife or health care provider can perform. So these formulas are recommended because they are simple, safe, low-cost, and acceptable methods for estimating fetal weight [9, 10].
Ultrasonography estimation of fetal weight is 20% more or less inconsistent with actual fetal weight, and this can lead to both false-positive and false-negative results in the third trimester of pregnancy [5, 11]. However, one study reported that all ultrasound formulas were highly accurate in fetal weight estimation, with only a 10% significant difference from the actual birth weight [12]. Another study reported the 100% sensitivity and 97.1% specificity of ultrasound in IUGR diagnosis, and its 48.1% sensitivity is, and 97.3% specificity in macrosomia diagnosis. Many researchers report that ultrasonography is as accurate as clinical methods in fetal weight estimation, and many studies say there are differences in this issue [13, 14, 15]; therefore, the role of clinical methods for EFW should be considered.
Another study reported that Insler’s formula is better in estimating fetal weight, while the results of another study showed that Johnson’s formula is more suitable [16]. In reports with a difference of ±500 g compared to the actual birth weight, the abdominal palpation’s sensitivity was 35.42%, Johnson’s formula 64.65%, Insler’s formula 67.68%. Also, the abdominal palpation’s specificity was 76%, Johnson’s formula 32.38%, and Insler’s formula 35.05%. When the difference was ±1000 g, the sensitivity of abdominal palpation was 20%, Johnson’s formula 50%, Insler’s formula 42.86%. Also, the abdominal palpation’s specificity was 94.33%, Johnson formula 52.03%, and Insler’s formula 54.73% [17, 18, 19].
Different methods are available for fetal weight estimation. A method with the lowest error and the highest accuracy is more suitable. So considering the importance of EFW and known complications of incorrect fetal weight estimation, the use of methods that are easy, inexpensive, and cost-effective is needed, especially in developing countries. Since delivery is not always done in the hospital, and many deliveries are done in deprived areas that do not have enough facilities, the importance of clinical methods becomes greater. Because of the cost of ultrasonography and its unavailability in many regions, it is essential to optimize diagnostic-treatment costs and present a suitable objective. This study was done to ensure the accuracy of clinical methods for EFW with Actual Birth Weight (ABW) in term pregnant women.
Materials and Methods
The present study is an assessment of the accuracy of diagnostic tests. The study was conducted from May to July 2018. According to a study of Haji Esmaeilou with a 95% confidence level, the Mean±SD weight was 1599/41 [20], and the acceptable amount of estimating error of 5%, we need 247 people. The methods used in this study were abdominal palpation, Johnson’s formula, Insler’s formula, and ultrasonography. The inclusion criteria included singleton pregnancy, gestational age of 37-41 weeks, and cephalic presentation. The exclusion criteria included the rupture of membranous, congenital malformation, and stillbirth.
Fetal weight by Insler’s formula was estimated by (weight in gr)=abdominal girth (cm) X symphysis fundal height (cm). Measurements are done by a tape measure of the Seca strip (German-made) with a precision of 1 mm. In measuring the height of the uterus, the distance between the upper extremity of the uterus and the upper edge of the symphysis of the pubis was considered to be zero points in the area of the symphysis of the pubis, and the strip meter stretched to the midline of the abdomen to the uterus and somewhere when the uterine peak was touched by the fingers; the height of the womb was measured in cm. To measure the abdominal circumference of the mother, the strip of the membrane in the position of the umbilicus passed through the abdomen and behind the mother, and the corresponding number was recorded in cm [6, 9, 10].
Fetal weight by Johnson’s formula was estimated by fetal weight (gr)=(symphysis fundal height - N)×155. In this formula, if the mother’s weight is over 90 kg, 1 cm of the height of the uterus is reduced. Also, for the calculation of N, the vaginal examination is performed: when the presenting part is at the minus station, N=13; presenting part was at ‘zero’ station, N=12; and presenting part was at plus station N=11. In measurements, the examination was done between contractions [6, 9].
The samples were followed up until delivery. The birth weight was measured by the Beurer digital scale (Germany) accurately 5 gr the first 24 hours of childbirth. The researcher carried a scale between the delivery room and the operating room when estimating the actual birth weight of the newborns. After obtaining written consent and recording the individual data, the weight and height of the mothers were measured. Then, in all clinical methods, after urination, the mother was placed in the supine position without knee bending. In this study, there was no limitation in delivery phases, both in the latent phase and in the active phase in the third trimester.
All clinical fetal weight measurements, including abdominal palpation, Johnson’s formula, Insler’s formula, were performed by a midwife (researcher) with at least two years of experience in obstetrics. The present study was conducted over three months. During this period, 700 pregnant women were referred to the therapeutic, educational center of the study environment, of which 400 were available, and among them, 247 pregnant women with inclusion criteria were examined.
All statistical analysis was performed in SPSS version 21. One-sample t-test, the Chi-square, and the Bland-Altman plot were used to compare the diagnostic value of fetal weight estimation methods. The difference between the fetal weight and the actual birth weight in all methods was considered significant when P <0.05 with the 1-sample test. For the error rate of methods with the difference was ±100 gr, the Chi-square test was used, and the accuracy of the studied methods was based on sensitivity and specificity in the classification of birth weights: below 2500 gr (low birth weight), 2500-4000 gr (normal birth weight) and above 4000 gr (high birth weight).
Results
The study results showed that the participating pregnant women had a Mean±SD age of 28.86±42.4 years (ranged 16-41 years), Mean±SD BMI of 32.98±6.0 kg/m2, and the Mean±SD gestational age of 39±1.04 weeks (ranged 37-41 weeks). The majority of women were multiparous (59.5%). The gender of the infant in the majority was male (52.6%), and the type of delivery in the majority was cesarean section (60.3%).
In the present study, the Mean±SD birth weight by clinical palpation was 3371.053±345.56 g, Mean±SD birth weight by Johnson’s was 3041.206±411.41 gr, Mean±SD birth weight with Insler’s was 3556.316±531.56) gr, Mean±SD birth weight by ultrasonography was 3294.28±380.0 gr, and Mean±SD actual birth weight was 3343.352±432.79) gr (Table 1).
.jpg)
One-sample t-test showed that abdominal palpation (P=0.261) and ultrasonography (P=0.118) were not significantly different with actual birth weight, but Johnson’s formula (P=0.001) and Insler’s formula (P=0.001) were significantly different with actual birth weight (Table 2).
.jpg)
In the group of the fetal weight of below 2500 gr, the Insler’s formula was more accurate in estimating fetal weight. In the normal weight range group, the highest accuracy belonged to Johnson’s formula, and at weights above 4000 gr, the abdominal palpation method was a better predictor in the estimation of fetal weight (Table 3).
.jpg)
In this study, the Bland-Altman plot indicated that the difference in fetal weight with actual birth weight in abdominal palpation and ultrasonography had no significant statistical difference, but there was a statistical difference with Johnson’s and Insler’s methods (Figures 1, 2, 3, 4).
This showes that abdominal palpation and ultrasonography methods as accurate as in the estimation of fetal weight.
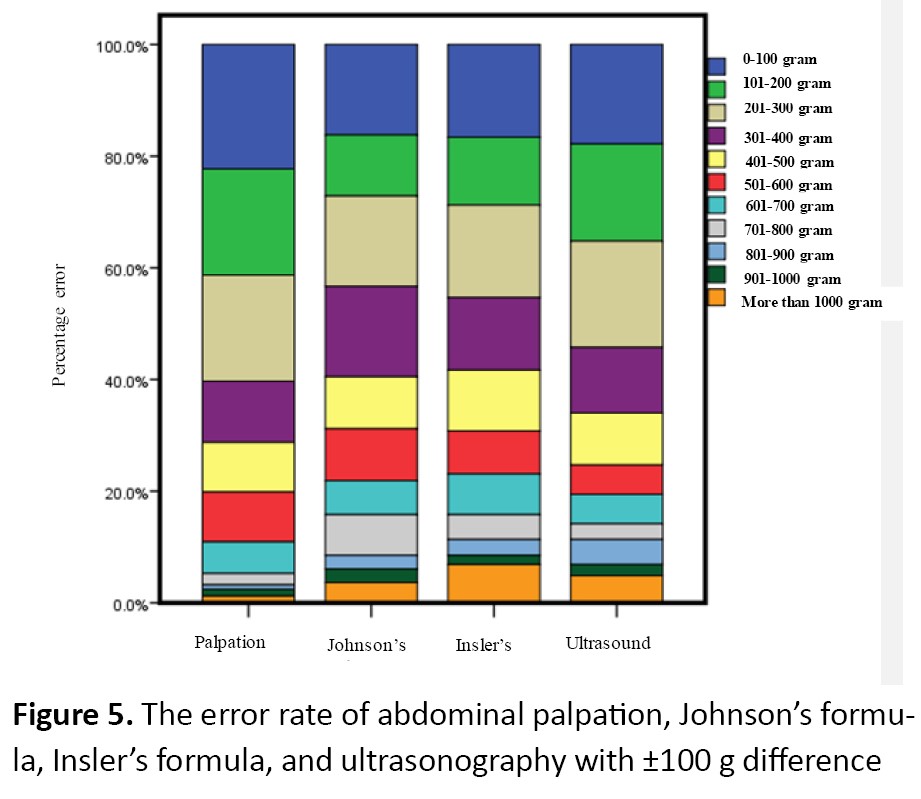
The Chi-square test showed a significant difference between clinical methods with actual birth weight. When the difference is fewer than 300 gr, maximum error belonged to abdominal palpation and minimum error to Johnson’s and Insler’s formulas. When the difference was more than 400 gr, a minimum error belonged to the abdominal palpation (Figure 5).
The Chi-square test showed a significant difference between clinical methods with actual birth weight. When the difference is fewer than 300 gr, maximum error belonged to abdominal palpation and minimum error to Johnson’s and Insler’s formulas. When the difference was more than 400 gr, a minimum error belonged to the abdominal palpation (Figure 5).
Discussion
The accurate prediction of fetal weight is an essential parameter in planning proper management of delivery. In the present study, according to the research results, the lowest difference between the mean fetal weight and the actual birth weight belonged to abdominal palpation, ultrasound, Johnson’s, and Insler’s, respectively.
In the present study, there is a significant difference between the Insler’s and Johnson’s formulas with the actual birth weight. Whereas by palpation and ultrasonography, the result is closer to the actual birth weight. The study results showed that the Insler’s and Johnson’s formulas had a statistically significant difference with the actual birth weight, but ultrasonography did not show any significant difference [21]. In another study, the estimation of fetal weight with ultrasonography was better than Insler’s and Johnson’s methods [11]. At the same time, several studies show that Johnson’s and Insler’s formulas had no significant difference with the actual birth weight [9, 22]. The probable reason for the inconsistency of current research with many studies may be the method, sample size, research environment, and sociocultural factors.
In our study, the actual birth weight was greater than the estimated weight by Insler’s method and less than the estimated weight by abdominal palpation. Some studies have shown that the least difference with actual birth weight was made by the Insler’s formula and the most difference by Johnson’s formula [10, 16]. The inconsistency of the present study with other studies was related to different sample sizes, percentage of error, inclusion and exclusion criteria, and statistical tests.
The present study showed that in estimating the fetal weight below 2500 gr, Insler’s method was better than other methods in LBW detection, which is similar to Sereke et al. research [12]. While in many studies, ultrasonography is better in low birth weight diagnosis [16, 18]. Also, in one study, Insler’s formula less accurately predicted low birth weight babies [22]. In the fetal weight group between 2500-4000 gr, the abdominal palpation had the highest accuracy, consistent with some studies [23, 24]. However, in many studies on the normal weight range, the ultrasound Insler’s formula is a better method to estimate fetal weight which the results of the present study are not in line with those findings [22, 25, 26]. Also, in the present study, fetuses with birth weights more than 4000 gr had the highest accuracy in estimating fetal weight by abdominal palpation. One study showed that the accuracy of the abdominal touch method was higher [19].
Other studies also showed that Insler’s and Johnson’s formulas and ultrasound are more accurate in macrosomia detection [12, 14, 27, 28]. Also, one study reported that with increasing gestational age and fetal weight, ultrasound error is less in estimating fetal weight [29]. The reason for the difference between the present study and other studies may be related to the estimated fetal weight by a midwife in the present study, while in many studies, different people estimated the fetal weight. Also, in the present study, fetal weight was estimated with different ultrasound devices, but in contradictory studies, pre-ultrasounds were performed by one device in one center.
The present study results showed that ultrasound results were not significantly different with actual birth weight, but Johnson’s and Insler’s formulas were significantly different with actual birth weight. Ultrasonography is as accurate as clinical methods in fetal weight estimation, which is consistent with some studies [30, 31]. In the present study, with a difference of fewer than 300 gr, the most error was reported by the abdominal palpation and the least by Johnson’s formula, and then by Insler’s formula. A study showed that Johnson’s formula with a difference of less than 300 gr has the highest accuracy [9]. In another study, Johnson’s formula is not suitable for estimating fetal weight in the Ethiopian population [32]. The possible reason for different results of studies may be related to racial differences, research method, statistical test, and sample size. In this study, with a difference of more than 300 gr, the lowest percentage error belonged to abdominal palpation. This finding indicates that by increasing the difference of fetal weight with birth weight, abdominal palpation and, by reducing the difference in fetal weight with the actual birth weight, the Insler’s and Johnson’s formula predicts better fetal weight.
The results of the present study and other studies [9, 15, 22, 33] indicate that clinical methods are essential in the estimation of fetal weight and suggest a method for the estimation of fetal weight. However, ultrasonography is the most common method for estimating fetal weight compared to clinical methods, but a gold standard has not yet been reported as the actual birth weight. This study showed that abdominal palpation is as accurate as ultrasonography in estimating fetal weight, and abdominal palpation can be used if ultrasonography is not available. This study also showed that Insler’s formula in identifying the LBW fetus and abdominal palpation in macrosomia diagnosis has better results than other methods. The study results indicate a similar result in the estimation of fetal weight between abdominal palpation and ultrasonography.
However, Insler’s formula was more accurate in detecting LBW and abdominal palpation in macrosomia. Clinical methods are accessible, available, cost-effective, and valuable that can be used to estimate fetal weight. In the present study, several ultrasound specialists have estimated the weight of the fetus by ultrasonography with different devices, and it is a limitation of the study. The strength of the research was the only researcher estimated the weight of the fetus with the abdominal touch technique in this study. Because of the limitations of the present study on the use of various ultrasound specialists, it is suggested that studies be conducted with the same purpose and by removing the above limitation.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the ethics committee of the Deputy of Research and Technology of Guilan University of Medical Sciences (Code: IR.GUMS.REC.2018.34).
Funding
The article was supported by Guilan University of Medical Sciences, Rasht, Iran.
Author's contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
The accurate prediction of fetal weight is an essential parameter in planning proper management of delivery. In the present study, according to the research results, the lowest difference between the mean fetal weight and the actual birth weight belonged to abdominal palpation, ultrasound, Johnson’s, and Insler’s, respectively.
In the present study, there is a significant difference between the Insler’s and Johnson’s formulas with the actual birth weight. Whereas by palpation and ultrasonography, the result is closer to the actual birth weight. The study results showed that the Insler’s and Johnson’s formulas had a statistically significant difference with the actual birth weight, but ultrasonography did not show any significant difference [21]. In another study, the estimation of fetal weight with ultrasonography was better than Insler’s and Johnson’s methods [11]. At the same time, several studies show that Johnson’s and Insler’s formulas had no significant difference with the actual birth weight [9, 22]. The probable reason for the inconsistency of current research with many studies may be the method, sample size, research environment, and sociocultural factors.
In our study, the actual birth weight was greater than the estimated weight by Insler’s method and less than the estimated weight by abdominal palpation. Some studies have shown that the least difference with actual birth weight was made by the Insler’s formula and the most difference by Johnson’s formula [10, 16]. The inconsistency of the present study with other studies was related to different sample sizes, percentage of error, inclusion and exclusion criteria, and statistical tests.
The present study showed that in estimating the fetal weight below 2500 gr, Insler’s method was better than other methods in LBW detection, which is similar to Sereke et al. research [12]. While in many studies, ultrasonography is better in low birth weight diagnosis [16, 18]. Also, in one study, Insler’s formula less accurately predicted low birth weight babies [22]. In the fetal weight group between 2500-4000 gr, the abdominal palpation had the highest accuracy, consistent with some studies [23, 24]. However, in many studies on the normal weight range, the ultrasound Insler’s formula is a better method to estimate fetal weight which the results of the present study are not in line with those findings [22, 25, 26]. Also, in the present study, fetuses with birth weights more than 4000 gr had the highest accuracy in estimating fetal weight by abdominal palpation. One study showed that the accuracy of the abdominal touch method was higher [19].
Other studies also showed that Insler’s and Johnson’s formulas and ultrasound are more accurate in macrosomia detection [12, 14, 27, 28]. Also, one study reported that with increasing gestational age and fetal weight, ultrasound error is less in estimating fetal weight [29]. The reason for the difference between the present study and other studies may be related to the estimated fetal weight by a midwife in the present study, while in many studies, different people estimated the fetal weight. Also, in the present study, fetal weight was estimated with different ultrasound devices, but in contradictory studies, pre-ultrasounds were performed by one device in one center.
The present study results showed that ultrasound results were not significantly different with actual birth weight, but Johnson’s and Insler’s formulas were significantly different with actual birth weight. Ultrasonography is as accurate as clinical methods in fetal weight estimation, which is consistent with some studies [30, 31]. In the present study, with a difference of fewer than 300 gr, the most error was reported by the abdominal palpation and the least by Johnson’s formula, and then by Insler’s formula. A study showed that Johnson’s formula with a difference of less than 300 gr has the highest accuracy [9]. In another study, Johnson’s formula is not suitable for estimating fetal weight in the Ethiopian population [32]. The possible reason for different results of studies may be related to racial differences, research method, statistical test, and sample size. In this study, with a difference of more than 300 gr, the lowest percentage error belonged to abdominal palpation. This finding indicates that by increasing the difference of fetal weight with birth weight, abdominal palpation and, by reducing the difference in fetal weight with the actual birth weight, the Insler’s and Johnson’s formula predicts better fetal weight.
The results of the present study and other studies [9, 15, 22, 33] indicate that clinical methods are essential in the estimation of fetal weight and suggest a method for the estimation of fetal weight. However, ultrasonography is the most common method for estimating fetal weight compared to clinical methods, but a gold standard has not yet been reported as the actual birth weight. This study showed that abdominal palpation is as accurate as ultrasonography in estimating fetal weight, and abdominal palpation can be used if ultrasonography is not available. This study also showed that Insler’s formula in identifying the LBW fetus and abdominal palpation in macrosomia diagnosis has better results than other methods. The study results indicate a similar result in the estimation of fetal weight between abdominal palpation and ultrasonography.
However, Insler’s formula was more accurate in detecting LBW and abdominal palpation in macrosomia. Clinical methods are accessible, available, cost-effective, and valuable that can be used to estimate fetal weight. In the present study, several ultrasound specialists have estimated the weight of the fetus by ultrasonography with different devices, and it is a limitation of the study. The strength of the research was the only researcher estimated the weight of the fetus with the abdominal touch technique in this study. Because of the limitations of the present study on the use of various ultrasound specialists, it is suggested that studies be conducted with the same purpose and by removing the above limitation.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the ethics committee of the Deputy of Research and Technology of Guilan University of Medical Sciences (Code: IR.GUMS.REC.2018.34).
Funding
The article was supported by Guilan University of Medical Sciences, Rasht, Iran.
Author's contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Stirnemann J, Salomon LJ, Papageorghiou A. The Intergrowth standards for Hadlock’s estimation of fetal weight. Ultrasound in Obstetrics & Gynecology. 2020; 56(6):946-8. [DOI:10.1002/uog.22000] [PMID]
- Mishra S, Ghatak S, Agrawal D, Singh P, Garg P. Estimation of fetal weight: An ultrasonography study in Indian population. Mymensingh Medical Journal: MMJ. 2020; 29(1):215-21. [PMID]
- Plonka M, Bociaga M, Radon-Pokracka M, Nowak M, Huras H. Comparison of eleven commonly used formulae for sonographic estimation of fetal weight in prediction of actual birth weight. Ginekologia Polska. 2020; 91(1):17-23. [DOI:10.5603/GP.2020.0005] [PMID]
- Lu Y, Fu X, Chen F, Wong KK. Prediction of fetal weight at varying gestational age in the absence of ultrasound examination using ensemble learning. Artificial Intelligence in Medicine. 2020; 102:101748. [DOI:10.1016/j.artmed.2019.101748] [PMID]
- Yazdani S, Boozari MS, Allah-Nazari M, Bijani A. [Comparison of fetal weight estimation with clinical, ultrasonographic methods, and combined formula of ultrasonography and maternal weight (Persian)]. The Iranian Journal of Obstetrics, Gynecology, and Infertility. 2014; 17(106):1-7. [10.22038/IJOGI.2014.3135]
- Razaq R. Comparison between clinical estimated fetal weights (CEFW) Versus Ultrasonographic estimated fetal weight (UEFW) for co-relation with actual birth weight (ABW) in 3rd Trimester of Pregnancy: Estimated Fetal Weights (CEFW) Versus Ultrasonographic Estimated Fetal Weight (UEFW). Annals of Gulf Medicine. 2020; 3(1):e1-4. [DOI:10.37978/gulf.v3i1.81]
- Cesnaite G, Domza G, Ramasauskaite D, Volochovic J. The accuracy of 22 fetal weight estimation formulas in diabetic pregnancies. Fetal Diagnosis and Therapy. 2020; 47(1):54-9. [DOI:10.1159/000500452] [PMID]
- Mossayebnezdad R, Niknami M, Pakseresht S. [Estimation of foetal weight by clinical examination and ultrasound methods in predicting actual birth weight: A narrative study (Persian)]. Indian Obstetrics and Gynaecology. 2019; 9(1):14-18. https://www.iog.org.in/index.php/iog/article/view/419.
- Sehrawat K, Panchanadikar TM. Johnson’s formula to compare fetal weight with actual birth weight. Indian Journal of Obstetrics and Gynecology Research. 2020; 7(2):147-52. [DOI:10.18231/j.ijogr.2020.031]
- Durgaprasad BK, Sharma S, Indira G. Comparative study between clinical methods and ultrasound examination in the estimation of fetal weight. International Journal of Health Sciences and Research. 2019; 9(5):79-86. https://www.ijhsr.org/IJHSR_Vol.9_Issue.5_May2019/13.pdf
- Acharya S, Tiwari A. Accuracy of prediction of birth weight by fetal ultrasound. Journal of KIST Medical College. 2020; 2(2):11-4. [DOI:10.3126/jkistmc.v2i2.33566]
- Sereke SG, Omara RO, Bongomin F, Nakubulwa S, Kisembo HN. Validation of sonographic fetal weight estimators among term parturients in Uganda. Research Square. 2020. [DOI:10.21203/rs.3.rs-103139/v1]
- Shen Y, Zhao W, Lin J, Liu F. Accuracy of sonographic fetal weight estimation prior to delivery in a Chinese han population. Journal of Clinical Ultrasound. 2017; 45(8):465-71. [DOI:10.1002/jcu.22463] [PMID]
- Dongol A, Bastakoti R, Pradhan N, Sharma N. Clinical estimation of fetal weight with reference to Johnson’s formula: An alternative solution adjacent to sonographic estimation of fetal weight. Kathmandu University Medical Journal. 2020; 18(70):111-6. [DOI:10.3126/kumj.v18i2.33219]
- Ravooru A, Gupta J, Anand AR. Comparative study of effective fetal weight by clinical formula with USG Hadlock formula. International Journal of Clinical Obstetrics and Gynaecology. 2020; 4(4):147-51. [DOI:10.33545/gynae.2020.v4.i4c.637]
- Malik R, Thakur P, Agarwal G. Comparison of three clinical and three ultrasonic equations in predicting fetal birth weight. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2016; 5(1):210-6. [DOI:10.18203/2320-1770.ijrcog20151627]
- Lanowski J-S, Lanowski G, Schippert C, Drinkut K, Hillemanns P, Staboulidou I. Ultrasound versus clinical examination to estimate fetal weight at term. Geburtshilfe und Frauenheilkunde. 2017; 77(3):276-83. [DOI:10.1055/s-0043-102406] [PMID] [PMCID]
- Bajaj P, Kadikar GK, Kannani M, Bhatt M, Shah S. Estimation of foetal birth weight clinically and sonographically and its correlation with its actual birth weight: A prospective and comparative study. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2017; 6(7):3103-8. [DOI:10.18203/2320-1770.ijrcog20172942]
- Weiner E, Mizrachi Y, Fainstein N, Elyashiv O, Mevorach-Zussman N, Bar J, et al. Comparison between three methods of fetal weight estimation during the active stage of labor performed by residents: A prospective cohort study. Fetal Diagnosis and Therapy. 2017; 42(2):117-23. [DOI:10.1159/000450944] [PMID]
- Haji Esmaeilou M, Mohamadi E. Comparison of the accuracy of clinical methods for estimation of fetal weight. International Journal of Medical Research & Health Sciences. 2016; 5(1):184-90. https://www.ijmrhs.com/abstract/comparison-of-the-accuracy-of-clinical-methods-for-estimation-of-fetal-weight-33.html
- Mgbafulu C, Ajah L, Umeora O, Ibekwe P, Ezeonu P, Orji M. Estimation of fetal weight: A comparison of clinical and sonographic methods. Journal of Obstetrics and Gynaecology. 2019; 39(5):639-46. [DOI:10.1080/01443615.2019.1571567.] [PMID]
- Ariyo BO, Yohanna S, Odekunle JO. Accuracy of the product of symphysio-fundal height and abdominal girth in prediction of birth weight among term pregnant women at Keffi, Nigeria. African Journal of Primary Health Care & Family Medicine. 2020; 12(1):e1-6. [DOI:10.4102/phcfm.v12i1.2113] [PMID] [PMCID]
- Ramaiah P, Elsayed LA, Lindsey G, Johargy A. Estimation of fetal size and weight using various formulas. International Journal of Trend in Scientific Research and Development. 2019; 3(3):991-4. [DOI:10.31142/ijtsrd23231 ]
- Ricchi A, Pignatti L, Bufalo E, De Salvatore C, Banchelli F, Neri I. Estimation of fetal weight near term: comparison between ultrasound and symphysis-fundus evaluation by Johnson’s rule. The Journal of Maternal-Fetal & Neonatal Medicine. 2019; 34(7):1070-4. [DOI:10.1080/14767058.2019.1623874] [PMID]
- Pradhan P, Neupane B, Shrestha S, Dangal G. Comparison of Johnson’s method with Hadlock’s method for estimation of fetal weight in term pregnancies. Journal of Nepal Health Research Council. 2019; 17(2):228-32. [DOI:10.33314/jnhrc.v0i0.1999.] [PMID]
- Shewly NR, Ferdous M, Begum H, Khan SH, Debee SR, Rahman S, et al. Discrepancy analysis between clinical versus ultrasound estimated fetal weight and actual birth weight at 3rd trimester. Journal of Shaheed Suhrawardy Medical College. 2019; 11(1):32-8. [DOI:10.3329/jssmc.v11i1.43176.]
- Abdalla HM. Accuracy of clinical methods for the estimation of fetal weight in single tone pregnancy at term at Iringa regional referral hospital. [MSc. thesis]. Tanzania: The University of Dodoma; 2019. http://41.78.64.25/handle/20.500.12661/2082
- Meyer R, Rottenstreich A, Tsur A, Cahan T, Shai D, Ilan H, et al. The effect of fetal weight on the accuracy of sonographic weight estimation among women with diabetes. The Journal of Maternal-Fetal & Neonatal Medicine. 2020:1-7. [DOI:10.1080/14767058.2020.1769592] [PMID]
- Castro-Vasquez BA, Taboada C. Accuracy of Estimated Fetal Weight in Third Trimester [33A]. Obstetrics & Gynecology. 2020; 135:16S-7. [DOI:10.1097/01.AOG.0000663068.01644.61]
- Njoku C, Emechebe C, Odusolu P, Abeshi S, Chukwu C, Ekabua J. Determination of accuracy of fetal weight using ultrasound and clinical fetal weight estimations in Calabar South, South Nigeria. International Scholarly Research Notices. 2014; 2014:970973. [DOI:10.1155/2014/970973] [PMID] [PMCID]
- Ingale A, Avinash Khade S, Shirodkar S. Clinical versus ultrasonographic fetal weight estimation and its correlation with actual birth weight. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2019; 8(2):503-12. [DOI:10.18203/2320-1770.ijrcog20190275]
- Yiheyis A, Alemseged F, Segni H. Johnson’s formula for predicting birth weight in pregnant mothers at Jimma University teaching hospital, South West Ethiopia. Medical Journal of Obstetrics and Gynecology. 2016; 4(3):1087. https://www.jscimedcentral.com/Obstetrics/obstetrics-4-1087.pdf
- Lertrat W, Kitiyodom S. Accuracy of intrapartum fetal weight estimation using dare’s formula and transabdominal ultrasonography in pregnant women with normal and high prepregnant BMI at Maharat Nakhon Ratchasima Hospital. Thai Journal of Obstetrics and Gynaecology. 2020. https://he02.tci-thaijo.org/index.php/tjog/article/view/242489
Article Type : Applicable |
Subject:
Special
Received: 2021/08/11 | Accepted: 2021/08/29 | Published: 2021/01/1
Received: 2021/08/11 | Accepted: 2021/08/29 | Published: 2021/01/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





.jpg)