Tue, Feb 3, 2026
Volume 35, Issue 3 (6-2025)
JHNM 2025, 35(3): 239-248 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Karimi F, Babazadeh R, Latifnejad Roudsari R, Asgharipour N, Esmaeeli H. The Effectiveness of Counseling Based on PLISSIT and BETTER Models on Postpartum Sexual Functioning in Women. JHNM 2025; 35 (3) :239-248
URL: http://hnmj.gums.ac.ir/article-1-1633-en.html
URL: http://hnmj.gums.ac.ir/article-1-1633-en.html
Farzane Karimi1 

 , Raheleh Babazadeh *2
, Raheleh Babazadeh *2 

 , Robab Latifnejad Roudsari3
, Robab Latifnejad Roudsari3 

 , Negar Asgharipour4
, Negar Asgharipour4 
 , Habibollah Esmaeeli5
, Habibollah Esmaeeli5 



 , Raheleh Babazadeh *2
, Raheleh Babazadeh *2 

 , Robab Latifnejad Roudsari3
, Robab Latifnejad Roudsari3 

 , Negar Asgharipour4
, Negar Asgharipour4 
 , Habibollah Esmaeeli5
, Habibollah Esmaeeli5 

1- Lecturer, Master’s (MSc) in Midwifery, Department of Midwifery, Faculty of Nursing and Midwifery Birjand Branch, Islamic Azad University, Birjand, Iran.
2- Department of Midwifery, Nursing and Midwifery Care Research Center, Mashhad University of Medical Sciences, Mashhad, Iran. ,babazadehr@mums.ac.ir
3- Assistant Professor, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Mashhad University of Medical Sciences, Mashhad, Iran
4- PhD in Clinical Psychology, Assistant Professor, Psychiatric and Behavioral Sciences Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
5- Social Determinants of Health Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
2- Department of Midwifery, Nursing and Midwifery Care Research Center, Mashhad University of Medical Sciences, Mashhad, Iran. ,
3- Assistant Professor, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Mashhad University of Medical Sciences, Mashhad, Iran
4- PhD in Clinical Psychology, Assistant Professor, Psychiatric and Behavioral Sciences Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
5- Social Determinants of Health Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
Full-Text [PDF 569 kb]
(268 Downloads)
| Abstract (HTML) (525 Views)
Full-Text: (224 Views)
Introduction
Sexual dysfunction in women is a growing problem in the world, which affects 10%–52 % of men and 25%–63 % of women. Women of reproductive age often suffer from sexual dysfunction and sexual dissatisfaction due to pregnancy, childbirth, breastfeeding, and infertility [1]. Female Sexual Dysfunction (FSD) affects approximately 40%–50% of women, irrespective of age [2]. One study states that over 78% of women resume vaginal sex by three months postpartum. By six months after delivery, 94% resume vaginal sex [3]. About 70.6% and 34.2% of women have sexual problems in the third and sixth postpartum months, respectively. Sexual dysfunction has been observed in 54.5% of the women at the 12th postpartum month [4, 5]. It should be noted that countless hormonal and physiological changes, as well as perineal traumas, types of delivery, and mental changes, can take place in the postpartum period, leading to sexual dysfunction [2, 6, 7]. Concerns about becoming pregnant again, breastfeeding, and vaginal delivery are factors that may postpone the resumption of sexual activity in some women. Despite the prevalence of this dysfunction, both physicians and women may delay talking about sexual concerns after pregnancy, and only 15% of women with postpartum sexual dysfunction have shared their problems with healthcare providers [8].
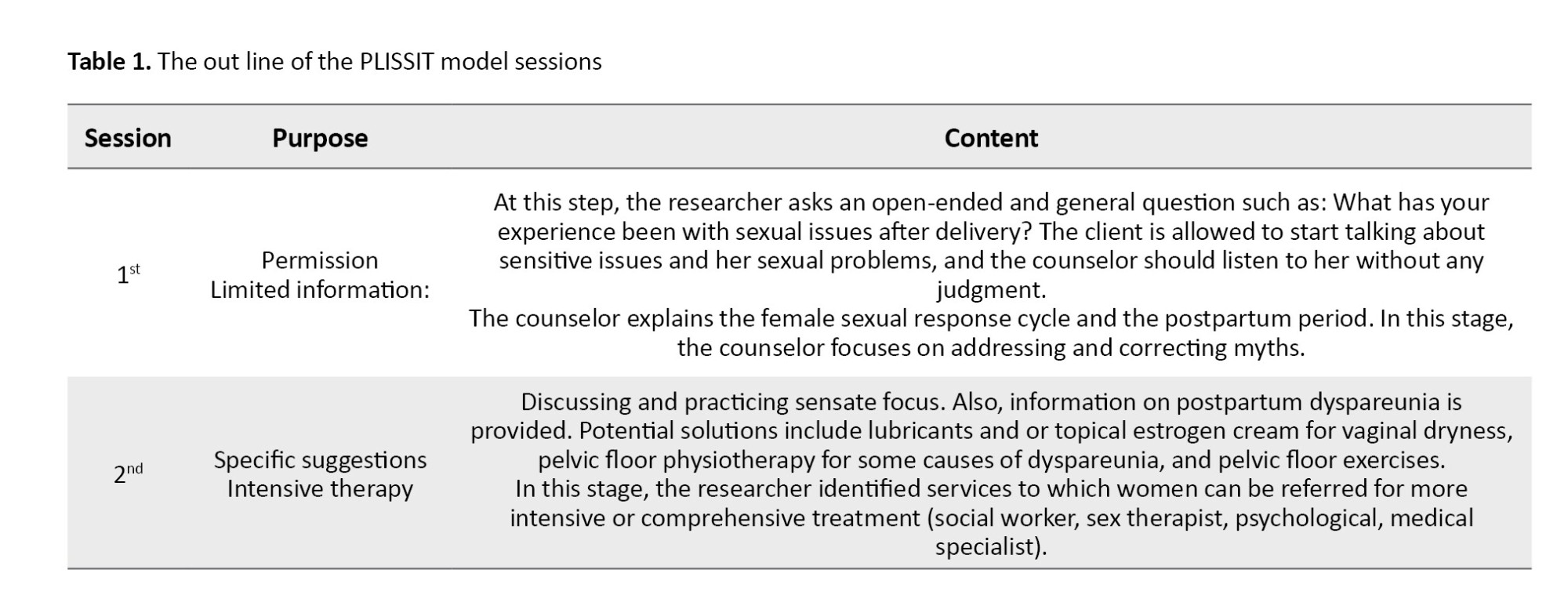
Various approaches have been designed for sexual counseling, including PLISSIT, which is known as one of the most commonly used models [9]. This model comprises 4 levels of intervention: Permission; Limited Information; Specific Suggestions; Intensive Therapy (PLISSIT) [10].
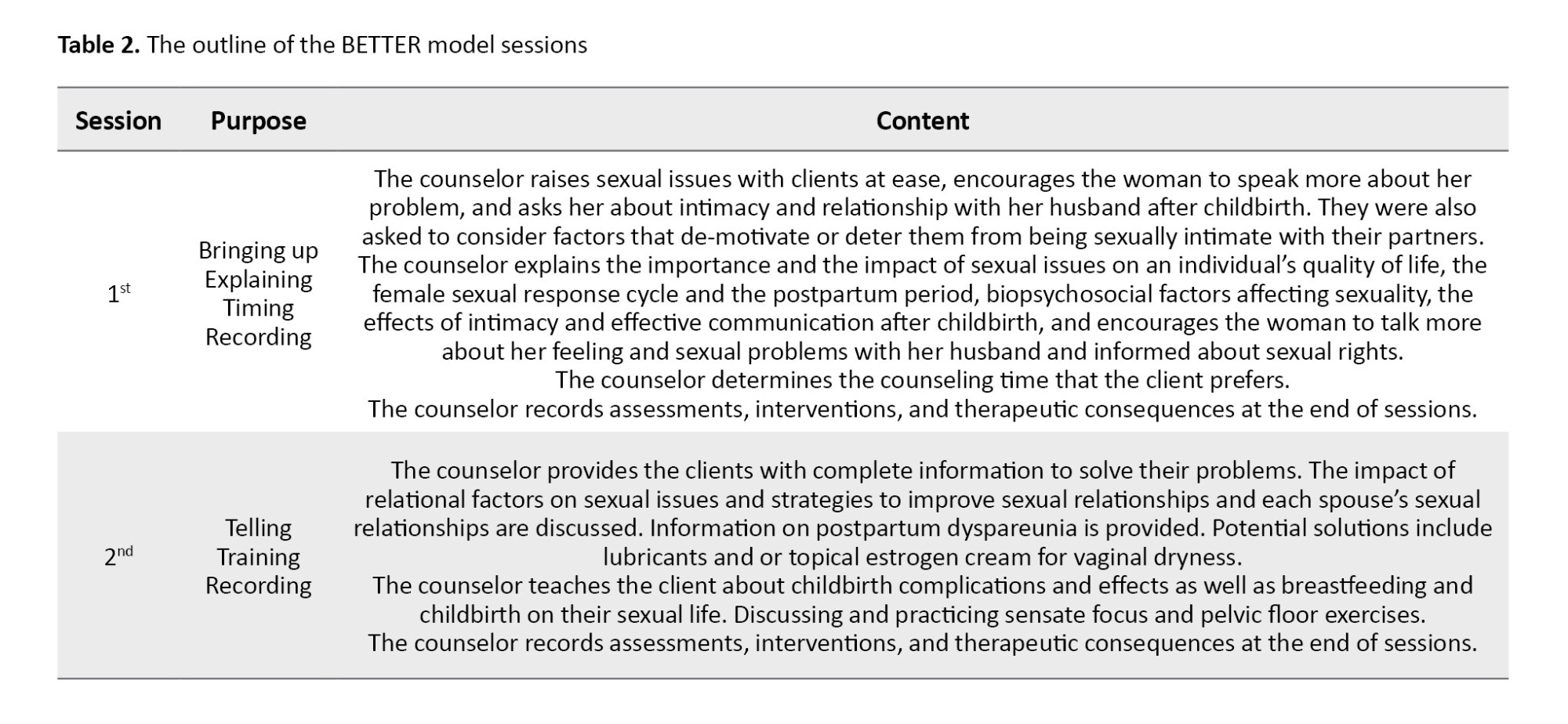
The BETTER model is used particularly for individuals affected with chronic diseases such as cancer and women in their postpartum period [11]. It is an attempt by experts to develop an instrument for improving dialogues about sexuality between clients and health care professionals, which can create a wider range of negotiations between counselors and clients based on individual timing and client information [12]. This model comprises six stages: Bringing Up, Explaining, Telling, Timing, Training, and Recording (BETTER) [11].
Because of special skills needed at the third and the fourth levels of the PLISSIT model, midwives and nurses are restrained in intervening at the first and second levels of this model. One of the limitations of this model is its linearity and proceeding from one level to the next, so the therapist cannot diagnose the necessity of returning to the previous level to fix the patient’s sexual concerns [10]. In the PLISSIT model, there is no chance of providing feedback to patients or healthcare professionals [13]. Ruling religious and cultural values in Iran make women not share their sexual dysfunction with counselors. Because research studies in this area have suggested the use of different counseling approaches to reduce women’s postpartum sexual dysfunction [10, 14, 15] and due to the lack of investigations conducted so far on comparing counseling approaches to reduce female postpartum sexual dysfunction, this study aimed to compare the effectiveness of counseling based on the standard PLISSIT model and the BETTER model, on postpartum sexual functioning in women after childbirth. We also intended to recommend using the most effective one for general postpartum counseling.
Materials and Methods
This research is a two-group, randomized, single-blind clinical trial. It was conducted on 90 women self-referring to 8 selected health care centers in Mashhad City, Iran, from March to August 2017. They reported sexual complaints within 4 weeks to 6 months after childbirth (normally, women from low to middle and high socioeconomic status get served at health care centers).
A random sampling method was used to select the health care centers. For this purpose, five large health care centers in Mashhad were considered, four of which (two urban and two rural) were selected using simple random sampling. Then, four urban health care centers were randomly selected from the list of the centers covered by each large center (eight centers in total), four of which were allocated to the BETTER group and four to the PLLISIT group with random allocation software. Next, the eligible subjects were selected from each center and assigned to the BETTER and PLLISIT groups. Finally, an informed consent form was obtained from each participant.
The inclusion criteria for this study were as follows: Iranian women being residents of Mashhad, being married and the only spouse of their husband; being 18-45 years old; being able to speak, read, and understand the Persian language; being healthy, singleton, and term newborn in recent childbirth; and obtaining scores equal to or less than 28 from Female Sexual Function Index (FSFI). The maximum score for each domain is 6, and the total index is 36. The appropriate cut-off point for the FSFI was determined to be equal to or less than 28 for the diagnosis of sexual dysfunction [16]. They should not have any sexual dysfunction before and during pregnancy, passed 4 weeks to 6 months of the postpartum period, resumed their sexual intercourse after delivery, lacked chronic diseases (diabetes mellitus, hypertension), alcohol abuse, or addiction to opioids and other psychoactive substances, obtained their scores of stress, anxiety, and depression less than 17, 9, and 13, respectively, according to the Depression Anxiety Stress Scales (DASS)-21, reported no diagnosis of mental and psychological problems such as severe depression, delirium, severe anxiety, and obsessive-compulsive disorder. Also, they should not suffer from late postpartum hemorrhage, postpartum infection, thromboembolic disorder, pelvic detachment, or mastitis based on their medical records. They should have a stable relationship with their husbands and no sexual disorders in their spouse. The exclusion criteria were becoming pregnant, breaking sexual intercourse, receiving comprehensive sex education, and consuming medications affecting their sexual functioning or that of their husband.
Pre-specified outcomes of the study were changes in the mean score of sexual function between two groups as measured by the FSFI before and 4 weeks after the intervention. There was no similar study in this regard; accordingly, the sample size was calculated at 38 individuals with 80% test power and 95% confidence interval to produce an effect size equal to 65%. However, the sample size was determined to be 45 patients in each group, considering a 20% sample loss.
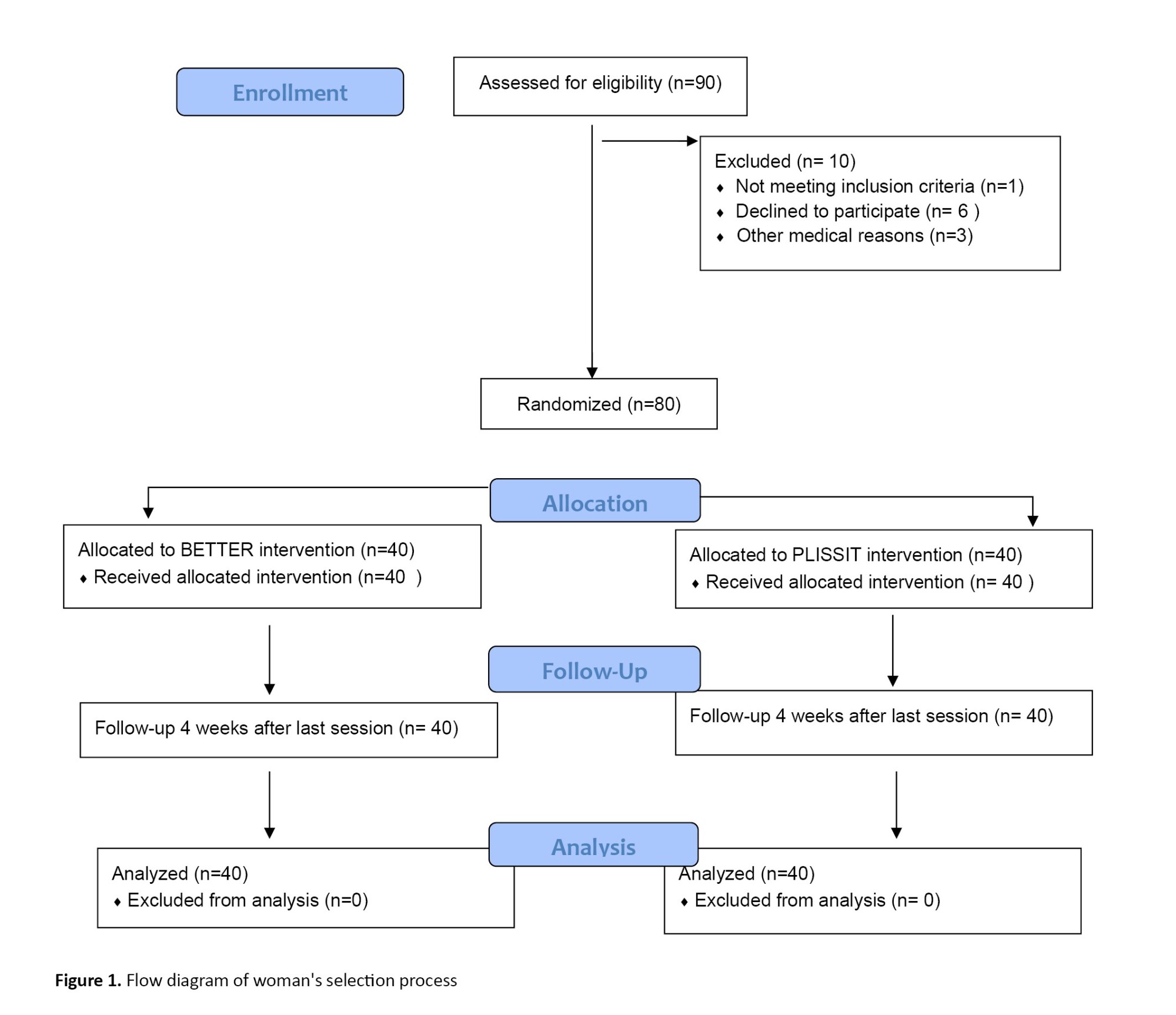
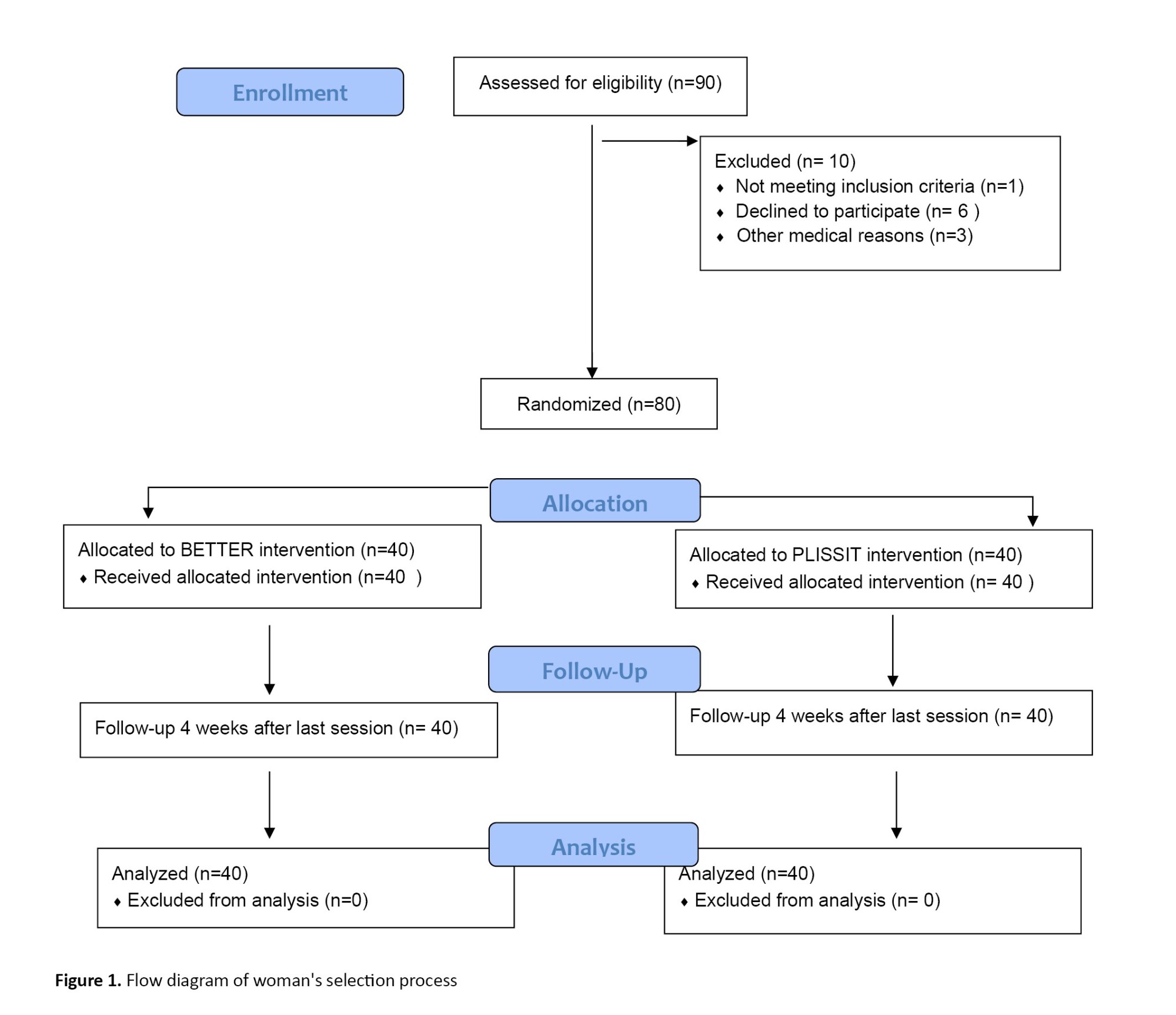
However, after the sample drop and exclusion (n=10) due to not meeting inclusion criteria (n=1), declining to participate (n=6), and other medical reasons (n=3), finally, 40 women in each group were assigned (Figure 1).
The data collection instruments included a demographic and sexual characteristics information questionnaire and the FSFI . The demographic and sexual characteristics information questionnaire contained 30 items prepared by the researchers. It was developed after reviewing the latest international books and articles on the topic of study, and its validity was also determined via content validity. So, after being prepared, it was submitted to 7 faculty members and professors at Mashhad University of Medical Sciences for checking its validity. The FSFI is a 19-item questionnaire designed to measure sexual functioning in women and assesses 6 domains of sexual function: Sexual desire, sexual arousal, lubrication, orgasm, satisfaction, and pain. Each item is rated on a 5-point scale. The participants answered each question according to their experiences. Questions 3 to 14 and 17 to 19 are scored 0-5, and questions 1, 2, 15, and 16 scored 1-5. Each domain’s scores are calculated by adding the scores of the individual items that comprise the domain, multiplying the sum by the domain factor (sexual desire 0.6, sexual arousal and lubrication 0.3, orgasm, satisfaction, and pain 0.4). The overall score range of maternal sexual performance was 2 to 36. The cut-off point of maternal sexual dysfunction was considered less than 28. The higher scores indicated better sexual performance validity and reliability of FSFI, which have been confirmed by Rosen et al. [17]. The present study used the psychometric version in Persian [16]. In the current study, the Cronbach α coefficient was estimated as 0.87.
Each random sequence generated was recorded on a card, and the cards were placed in non-transparent, sealed, and opaque envelopes, respectively. To preserve the random sequence, the outer surface of the envelopes was numbered in the same order. Finally, the envelopes were closed and placed in a box, and participants were assigned to one of the two groups (each group 40) respectively. Farzane Karimi enrolled participants and consulted with women, Negar Asgharipour created the random sequence and allocation concealment, and Raheleh Babazadeh assigned participants to interventions.
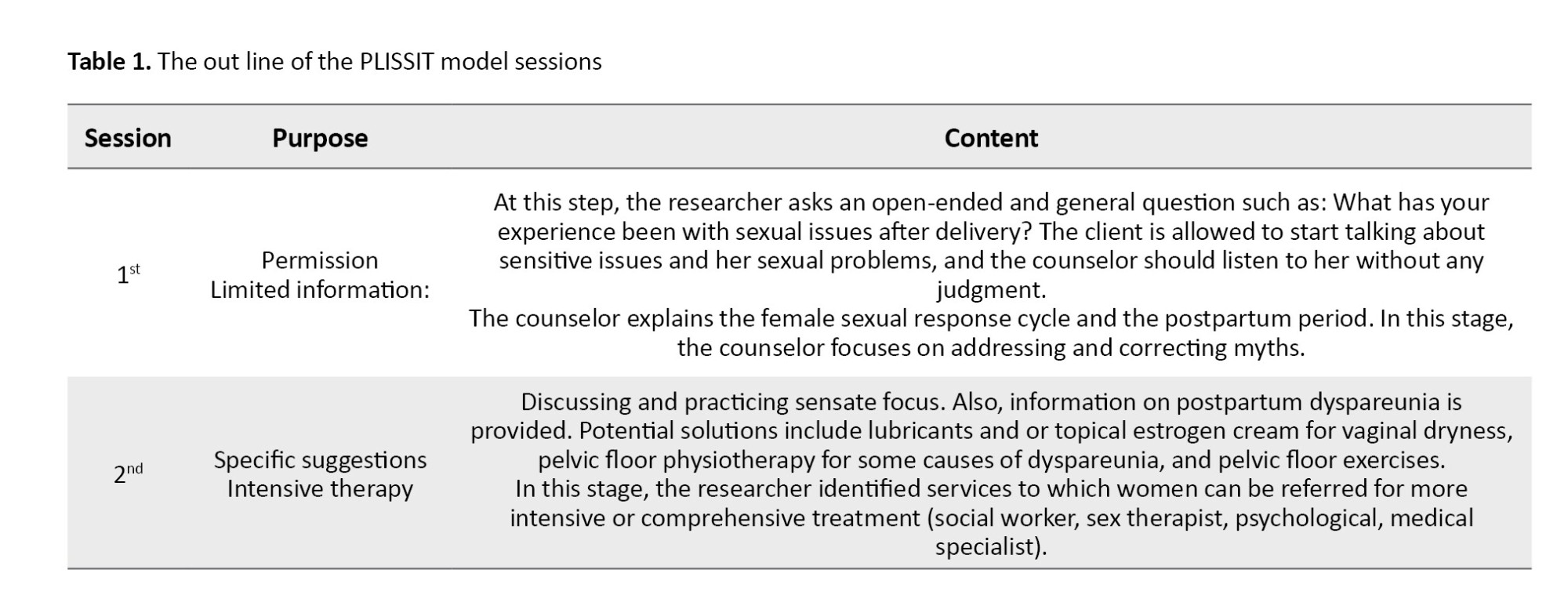
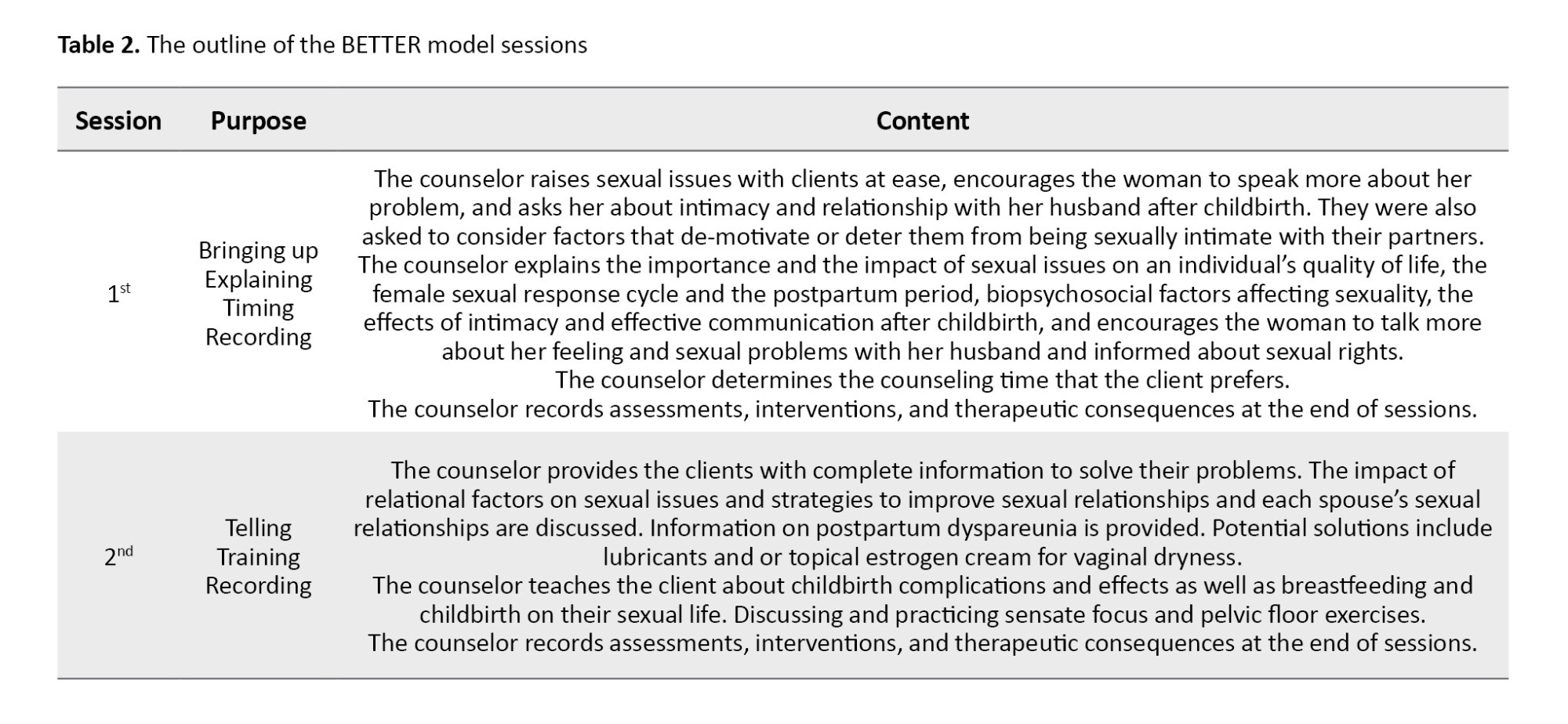
Women in both PLISSIT and BETTER groups attended two sessions and received individual consultations weekly for two weeks in the counseling room of the given center. Each session lasted 90 minutes. The consulting time was equal for all women in 2 groups (Tables 1 and 2). FSFI was assessed at the beginning and 4 weeks after the last session.
The statistical analyst was blinded to the study. After data collection, all data were analyzed using SPSS software, version 24 (IBM, Armonk, NY, USA). The Kolmogorov-Smirnov test was used to check the normality of values. Values are expressed as Mean±SD or number (percentage). The comparison of FSFI score between ‘pre-intervention versus post-intervention’ and ‘BETTER group versus PLISSIT group’ was performed using an independent t-test and analysis of covariance. The P<0.05 was considered significant.
Results
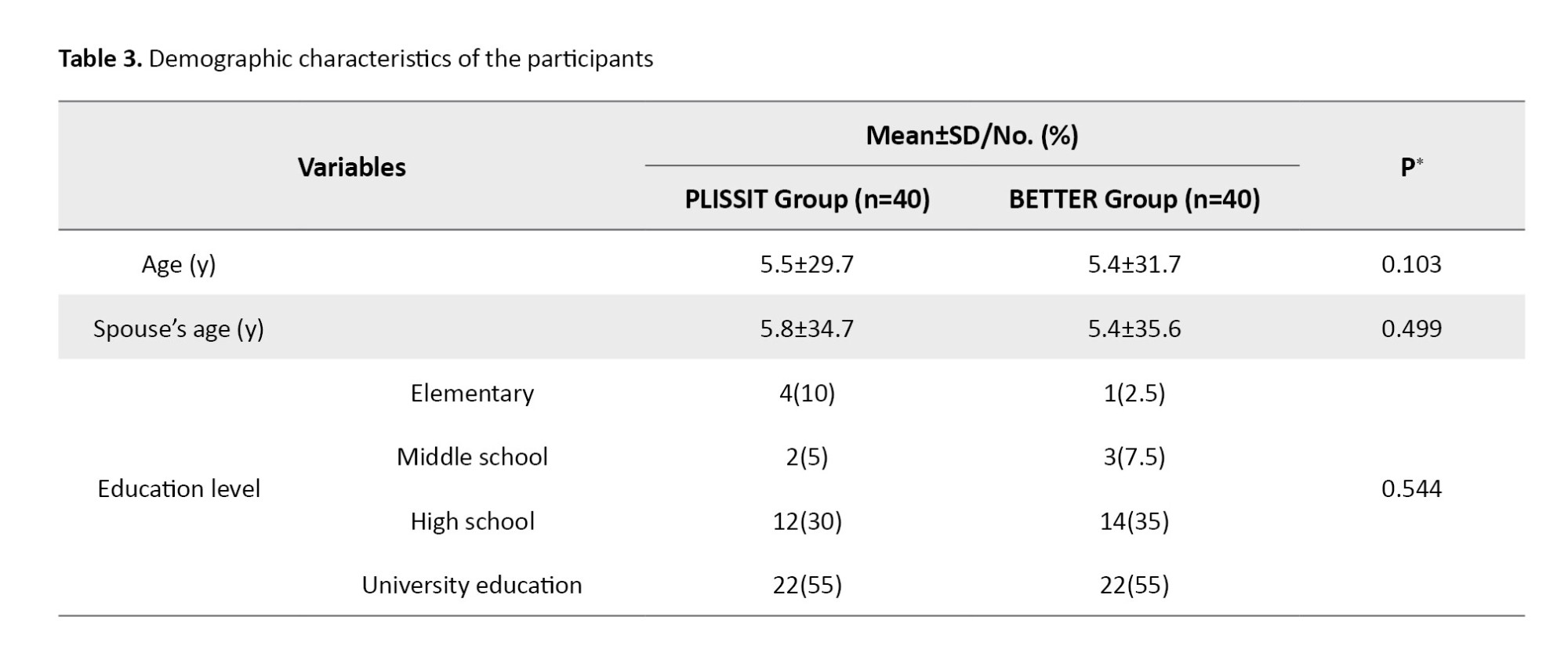
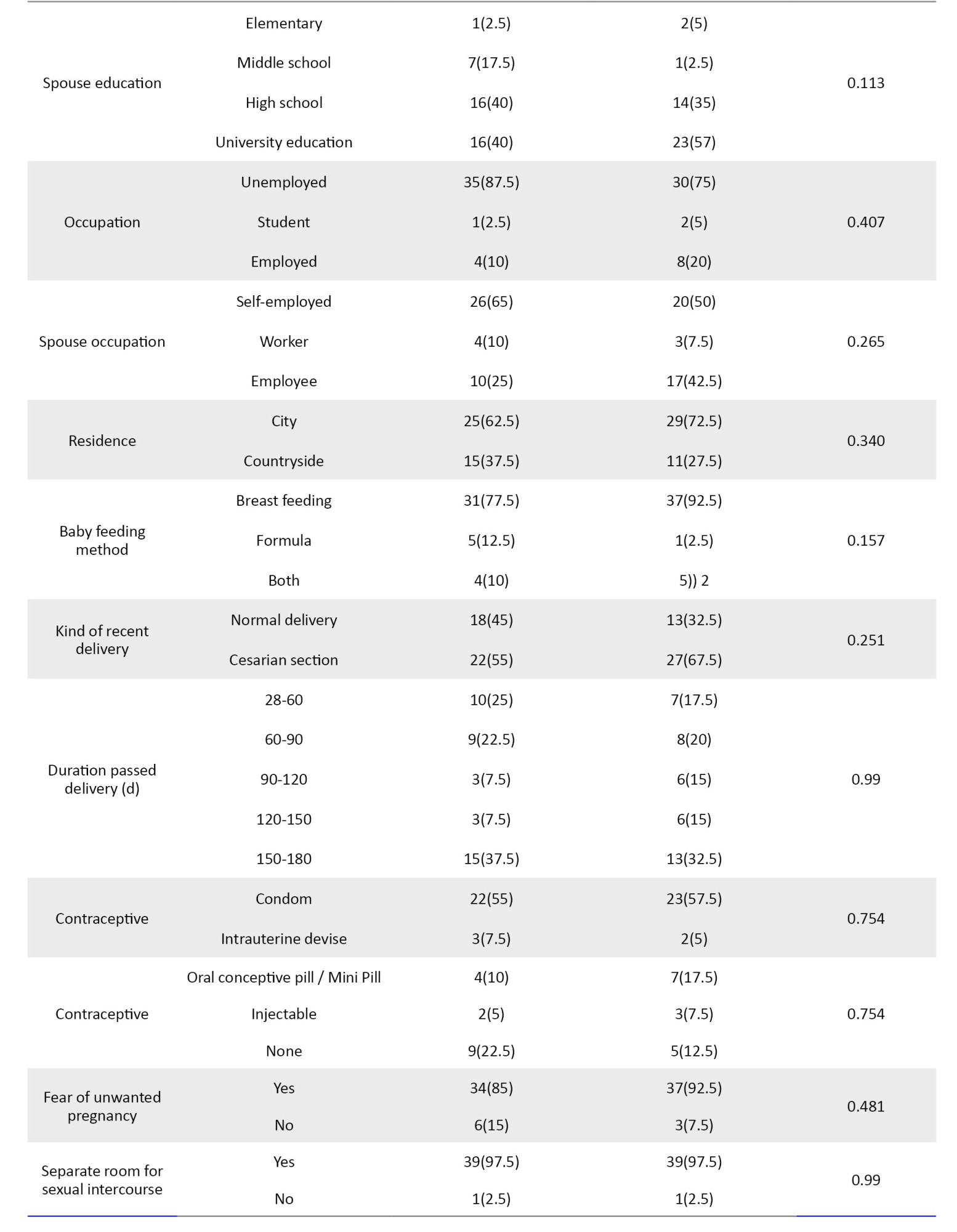
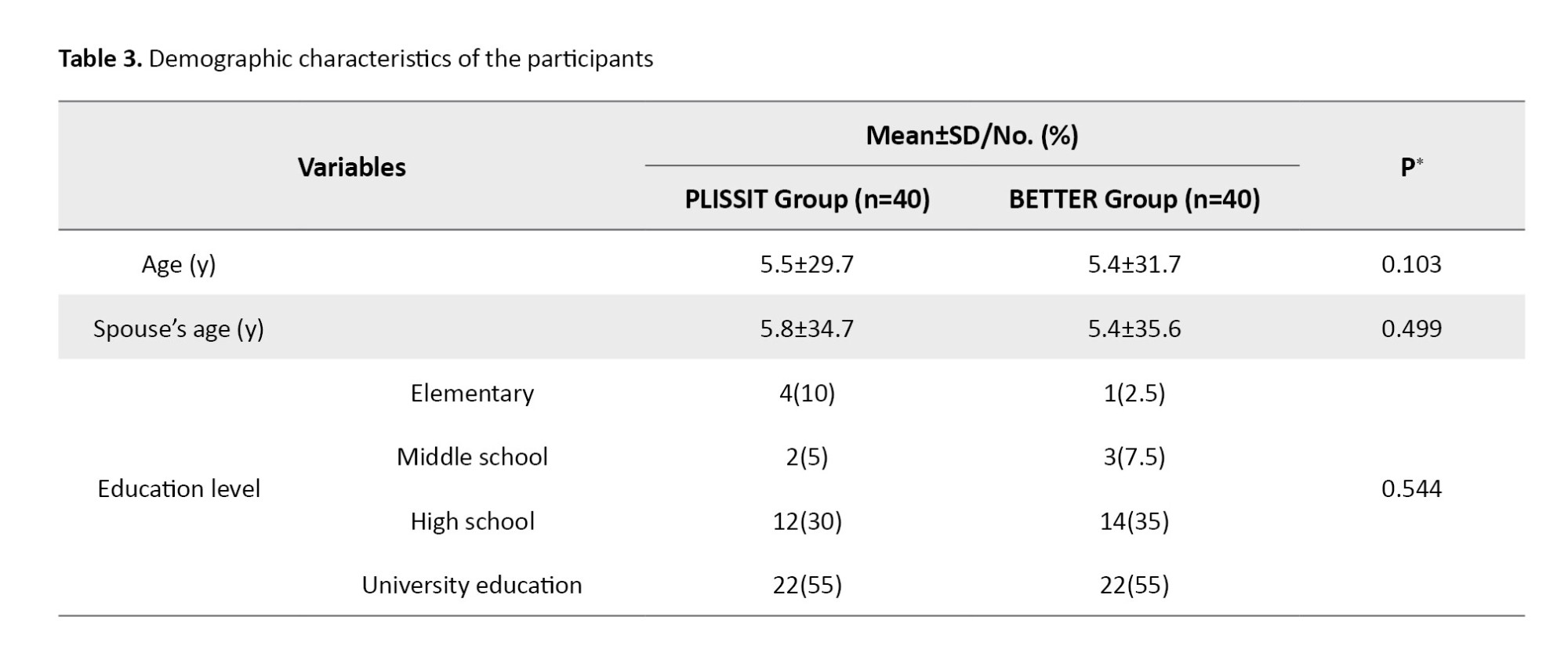
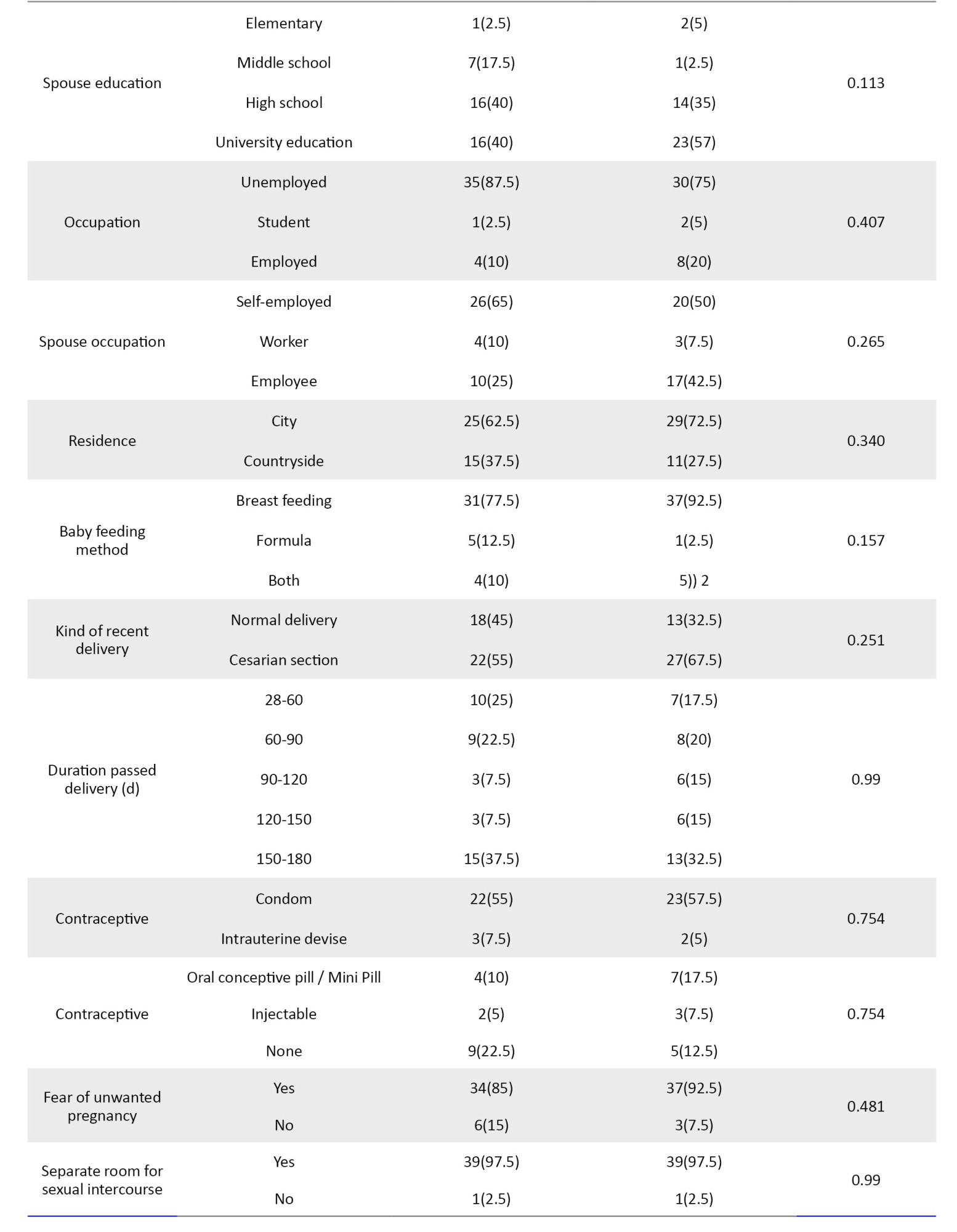
Demographic and sexual characteristics examined and compared before the intervention and between the two study groups were homogenous in all cases. The Mean±SD ages of women were 29.7±5.5 years in the BETTER group and 31.7±5.4 years in the PLLISIT group. The majority of participants in both groups were unemployed. The kind of recent delivery in most participants in the two groups was the cesarian section (55% in BETTER and 67.5% in the PLLISIT group). The majority of participants in both groups used condoms for preventing pregnancy, 55% in BETTER and 57.5% in PLLISIT (Table 3).
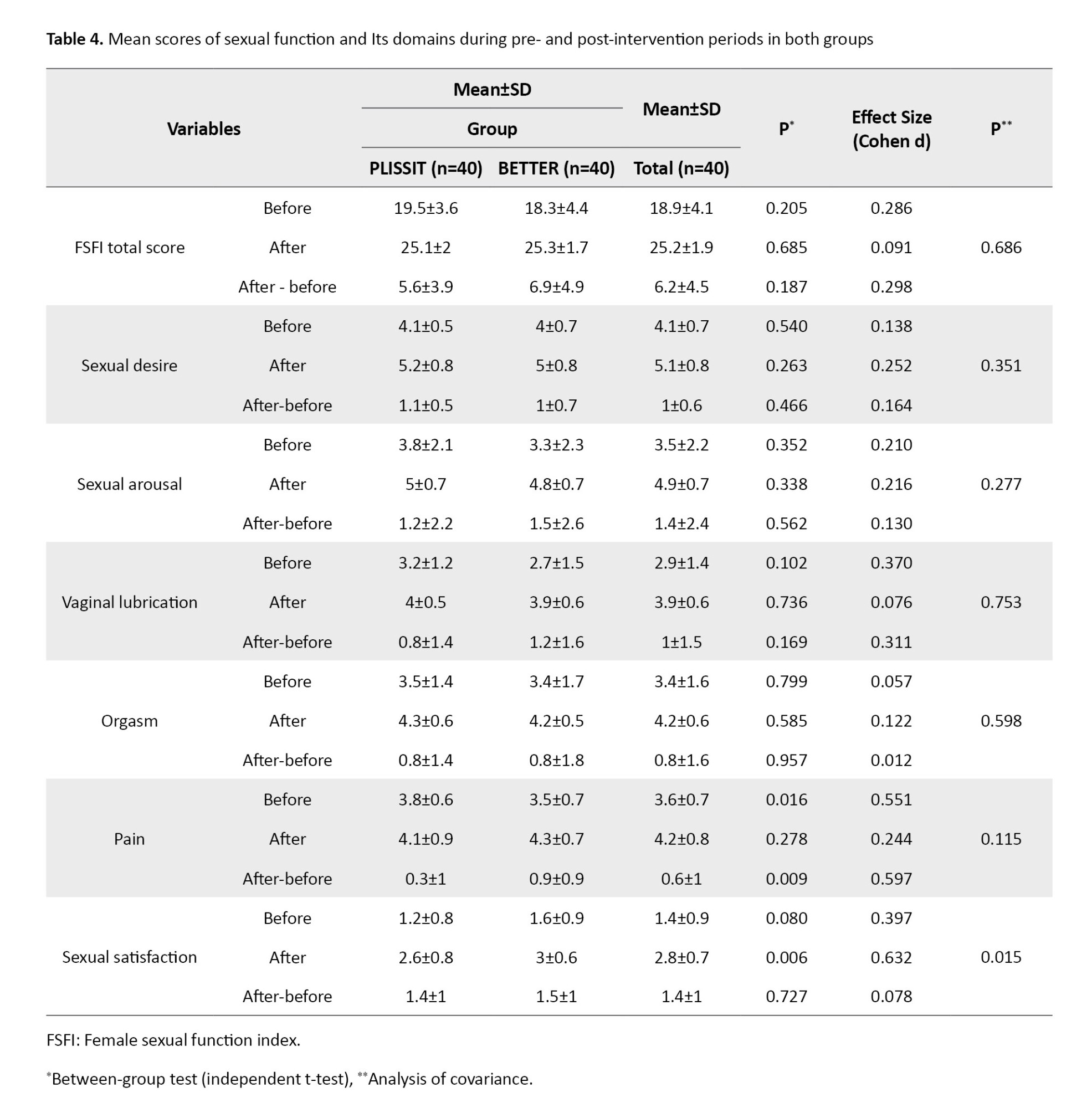
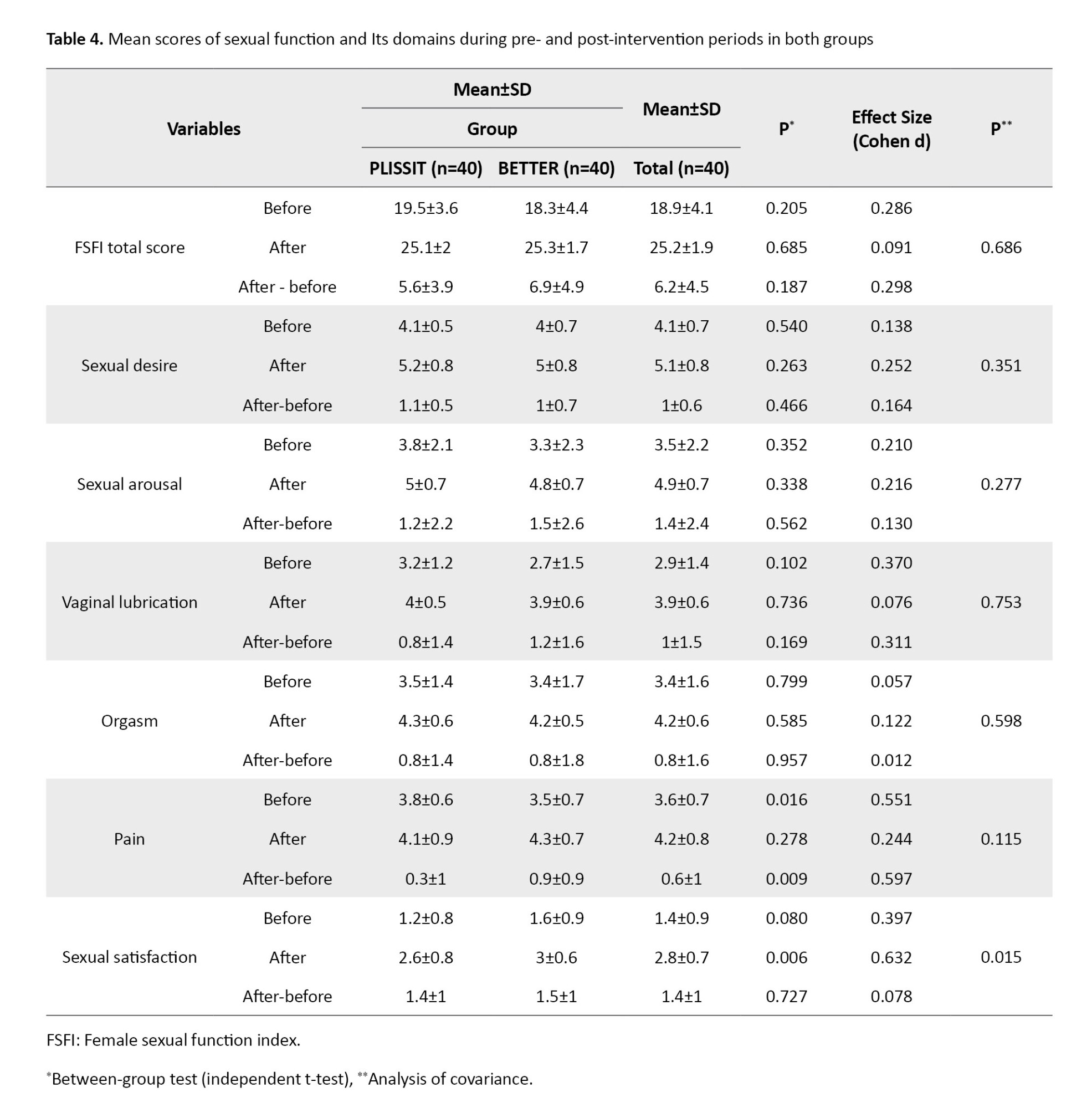
The Kolmogorov-Smirnov test showed normal distribution. An independent t-test was used to compare the scores of sexual functioning at each stage between the two groups. The FSFI mean total scores in the PLLISIT and BETTER groups before the intervention were 19.5±3.6 and 18.3±4.4, respectively. However, the FSFI mean total scores in the PLLISIT and BETTER groups after the intervention were 25.1±2.0 and 25.3±1.7, respectively. The effect of the group on sexual function scores was tested using covariance analysis and score control of each variable before the intervention. The covariance analysis showed that the impact of the group on orgasm, pain, sexual desire, sexual arousal, vaginal lubrication, and FSFI total score was not statistically significant. The sexual satisfaction change after the intervention in the BETTER group was significant (P=0.015). After the intervention, the score of this domain increased by 1.4±1.0 in the PLISSIT group and 1.5±1.0 in the BETTER group (Cohen d=0.078). These results are shown in Table 4.
Discussion
The purpose of this study was to compare the effectiveness of counseling based on the standard PLISSIT and BETTER models on postpartum sexual functioning in women after childbirth.
Sexual satisfaction in the PLLISIT and BETTER groups before the intervention was not significantly different. This randomized trial showed a significant increase in sexual satisfaction in women after the intervention. In the literature, we found no study regarding women’s use of the BETTER model intervention plan in their postpartum period. The results of the present study were compared with the findings of the studies carried out via different counseling approaches and their impacts on women’s sexual function during reproductive age or after childbirth.
We found that the effect of the group on orgasm, pain, sexual desire, sexual arousal, vaginal lubrication, and FSFI total score after the intervention was not statistically significant between PLISSSIT and BETTER models. Still, sexual satisfaction in the BETTER model was increased. In another study, it was found that the BETTER model is effective in the improvement of sexual functions and sexual satisfaction in women with one to two years of infertility [18]. Another study concluded that counseling using the PLISSIT model has a positive effect on the sexual satisfaction of women [19]. One study concluded that the PLISSIT model had no significant impact on sexual function after childbirth, and using other counseling approaches was suggested [20]. One study determined the effect of counseling on sexual functioning based on the PLISSIT model on 90 postpartum breastfeeding mothers 6 months after giving birth. The study found that sexual counseling based on the PLISSIT model was effective in promoting sexual functioning compared to the control group (no intervention) [9]. Although counseling based on the PLISSIT and sexual health models was effective in the improvement of sexual function, in one study, individual therapy (PLISSIT model) was more effective than group therapy with the sexual health model [15].
Also, in this study, a comparison of the mean scores of 6 domains of sexual function in the 2 intervention groups before and 4 weeks after the intervention showed a significant difference in just one domain of sexual satisfaction. The BETTER model helps women to express their sexual life problems and prepare an appropriate treatment environment for their sexual function problems [18]. In the BETTER model, the counselor starts a dialogue, clarifies the importance of sexual issues for clients, and encourages the women to talk more about their problems. In comparison with the PLISSIT model, the counselor tries to remove the taboo of talking about sexual concerns with the husband, which can act as an impetus to self-expression and self-disclosure. Consequently, the couples begin to remove the barriers to communicating about sex that can be effective in sexual arousal and satisfaction
The results of this study show that sexual desire, orgasm, and sexual lubrication had increased and pain decreased in both groups after the intervention, but the results were not significant; these findings are in line with 2 studies that utilized the PLISSIT model in sexual education or counseling [21, 22]. This discrepancy in the pain domain may be related to cultural and personal differences in pain perception between the populations studied since culture, personal experiences, and pain tolerance deeply influence pain sensation. Lee stated that women were likely to have less sexual desire in the postpartum period due to weakness, fatigue, breastfeeding, perineal pain, reduced vaginal lubrication, and fear of wound damage or unwanted pregnancy [23].
Some studies show that although most women having resumed vaginal intercourse by 12 weeks postpartum, 30% to 62% felt pain with sex [23, 24]. The result in the domain of orgasm was in line with Mabrouk et al. [25]. The most frequent sexual disorder after 9 months postpartum included orgasm (10.8%) [26]. However, our findings disagree with the results reported by Farnam et al. [15]. The reasons for this inconsistency result from differences in study samples, questionnaires, methodologies, and psychosocial, emotional, and cognitive factors involved in women’s orgasm [27].
It should be noted that the first orgasm following childbirth can occur after 7 weeks on average (at the range of 2-18 weeks), and during the first postpartum intercourse, only 20% of women can have an orgasmic experience, which can increase to 3-6 months after childbirth [24]. In a study by Behboodi Moghadam et al., utilizing 4 sessions of sexual education program over 4 weeks could improve the sexual score of all domains of FSFI in married women with sexual dysfunction [28]. Probably more sessions are needed to increase all domains of FSFI after childbirth, and women may need more than 6 months after delivery to return to their non-pregnant condition.
One of the strengths of this study was the innovative implementation of sexual counseling based on the BETTER model for the first time after childbirth. Since the counseling sessions were conducted one-on-one, a good sample size could be considered the other strength of this study.
Among the limitations of this study was the impossibility of assessing the sexual problems of women’s marriage partners (men), so their self-reports about the absence of a sexual problem in their husbands were included in this study. The study participants were women who had actively sought help for their sexual dysfunction and, therefore, may not be representative of all postnatal women.
A comparison of the scores between the two groups of this study showed overall differences in sexual satisfaction in the BETTER group. With an emphasis on a person-centered approach and sexual communication as well as determining counseling time tailored to the client’s preferences, the BETTER sexuality model could have a greater impact on sexual functioning in clients and increase their sexual satisfaction. It can be recommended that further studies should be performed on sexual counseling after postpartum to reveal their long-term outcomes.
Ethical Considerations
Compliance with ethical guidelines
This research project was approved by the Ethics Committee of Mashhad University of Medical Sciences, Mashhad, Iran (Code: IR.MUMS.REC.1396.160) and was registered by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20170430033718N3). It was assured that the participants’ information would be kept confidential. The data were coded and anonymized on the computer. The samples were assured that they would be presented with the study results if desired.
Funding
This study was extracted from the master’s thesis of Farzaneh Karimi, approved by the Department of Midwifery, Faculty Of Nursing and Midwifery, Mashhad University of Medical Sciences. This research was supported by the Research Deputy of Mashhad University of Medical Sciences, Mashhad, Iran (Code: 951749).
Authors' contributions
Conceptualization, study design, resources, review, and editing: Farzane Karimi, Raheleh Babazadeh, Robab Latifnejad Roudsari, and Negar Asgharipour; Investigation and writing the original draft: Farzane Karimi, Raheleh Babazadeh, and Robab Latifnejad Roudsari; Data collection: Farzane Karimi and Raheleh Babazadeh; Data analysis: Habibollah Esmaeeli; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors hereby appreciate the Vice-Chancellor’s Office for Research at Mashhad University of Medical Sciences for providing financial support for this study. The authors also thank all the women who participated in this research.
References
Sexual dysfunction in women is a growing problem in the world, which affects 10%–52 % of men and 25%–63 % of women. Women of reproductive age often suffer from sexual dysfunction and sexual dissatisfaction due to pregnancy, childbirth, breastfeeding, and infertility [1]. Female Sexual Dysfunction (FSD) affects approximately 40%–50% of women, irrespective of age [2]. One study states that over 78% of women resume vaginal sex by three months postpartum. By six months after delivery, 94% resume vaginal sex [3]. About 70.6% and 34.2% of women have sexual problems in the third and sixth postpartum months, respectively. Sexual dysfunction has been observed in 54.5% of the women at the 12th postpartum month [4, 5]. It should be noted that countless hormonal and physiological changes, as well as perineal traumas, types of delivery, and mental changes, can take place in the postpartum period, leading to sexual dysfunction [2, 6, 7]. Concerns about becoming pregnant again, breastfeeding, and vaginal delivery are factors that may postpone the resumption of sexual activity in some women. Despite the prevalence of this dysfunction, both physicians and women may delay talking about sexual concerns after pregnancy, and only 15% of women with postpartum sexual dysfunction have shared their problems with healthcare providers [8].
Various approaches have been designed for sexual counseling, including PLISSIT, which is known as one of the most commonly used models [9]. This model comprises 4 levels of intervention: Permission; Limited Information; Specific Suggestions; Intensive Therapy (PLISSIT) [10].
The BETTER model is used particularly for individuals affected with chronic diseases such as cancer and women in their postpartum period [11]. It is an attempt by experts to develop an instrument for improving dialogues about sexuality between clients and health care professionals, which can create a wider range of negotiations between counselors and clients based on individual timing and client information [12]. This model comprises six stages: Bringing Up, Explaining, Telling, Timing, Training, and Recording (BETTER) [11].
Because of special skills needed at the third and the fourth levels of the PLISSIT model, midwives and nurses are restrained in intervening at the first and second levels of this model. One of the limitations of this model is its linearity and proceeding from one level to the next, so the therapist cannot diagnose the necessity of returning to the previous level to fix the patient’s sexual concerns [10]. In the PLISSIT model, there is no chance of providing feedback to patients or healthcare professionals [13]. Ruling religious and cultural values in Iran make women not share their sexual dysfunction with counselors. Because research studies in this area have suggested the use of different counseling approaches to reduce women’s postpartum sexual dysfunction [10, 14, 15] and due to the lack of investigations conducted so far on comparing counseling approaches to reduce female postpartum sexual dysfunction, this study aimed to compare the effectiveness of counseling based on the standard PLISSIT model and the BETTER model, on postpartum sexual functioning in women after childbirth. We also intended to recommend using the most effective one for general postpartum counseling.
Materials and Methods
This research is a two-group, randomized, single-blind clinical trial. It was conducted on 90 women self-referring to 8 selected health care centers in Mashhad City, Iran, from March to August 2017. They reported sexual complaints within 4 weeks to 6 months after childbirth (normally, women from low to middle and high socioeconomic status get served at health care centers).
A random sampling method was used to select the health care centers. For this purpose, five large health care centers in Mashhad were considered, four of which (two urban and two rural) were selected using simple random sampling. Then, four urban health care centers were randomly selected from the list of the centers covered by each large center (eight centers in total), four of which were allocated to the BETTER group and four to the PLLISIT group with random allocation software. Next, the eligible subjects were selected from each center and assigned to the BETTER and PLLISIT groups. Finally, an informed consent form was obtained from each participant.
The inclusion criteria for this study were as follows: Iranian women being residents of Mashhad, being married and the only spouse of their husband; being 18-45 years old; being able to speak, read, and understand the Persian language; being healthy, singleton, and term newborn in recent childbirth; and obtaining scores equal to or less than 28 from Female Sexual Function Index (FSFI). The maximum score for each domain is 6, and the total index is 36. The appropriate cut-off point for the FSFI was determined to be equal to or less than 28 for the diagnosis of sexual dysfunction [16]. They should not have any sexual dysfunction before and during pregnancy, passed 4 weeks to 6 months of the postpartum period, resumed their sexual intercourse after delivery, lacked chronic diseases (diabetes mellitus, hypertension), alcohol abuse, or addiction to opioids and other psychoactive substances, obtained their scores of stress, anxiety, and depression less than 17, 9, and 13, respectively, according to the Depression Anxiety Stress Scales (DASS)-21, reported no diagnosis of mental and psychological problems such as severe depression, delirium, severe anxiety, and obsessive-compulsive disorder. Also, they should not suffer from late postpartum hemorrhage, postpartum infection, thromboembolic disorder, pelvic detachment, or mastitis based on their medical records. They should have a stable relationship with their husbands and no sexual disorders in their spouse. The exclusion criteria were becoming pregnant, breaking sexual intercourse, receiving comprehensive sex education, and consuming medications affecting their sexual functioning or that of their husband.
Pre-specified outcomes of the study were changes in the mean score of sexual function between two groups as measured by the FSFI before and 4 weeks after the intervention. There was no similar study in this regard; accordingly, the sample size was calculated at 38 individuals with 80% test power and 95% confidence interval to produce an effect size equal to 65%. However, the sample size was determined to be 45 patients in each group, considering a 20% sample loss.
However, after the sample drop and exclusion (n=10) due to not meeting inclusion criteria (n=1), declining to participate (n=6), and other medical reasons (n=3), finally, 40 women in each group were assigned (Figure 1).
The data collection instruments included a demographic and sexual characteristics information questionnaire and the FSFI . The demographic and sexual characteristics information questionnaire contained 30 items prepared by the researchers. It was developed after reviewing the latest international books and articles on the topic of study, and its validity was also determined via content validity. So, after being prepared, it was submitted to 7 faculty members and professors at Mashhad University of Medical Sciences for checking its validity. The FSFI is a 19-item questionnaire designed to measure sexual functioning in women and assesses 6 domains of sexual function: Sexual desire, sexual arousal, lubrication, orgasm, satisfaction, and pain. Each item is rated on a 5-point scale. The participants answered each question according to their experiences. Questions 3 to 14 and 17 to 19 are scored 0-5, and questions 1, 2, 15, and 16 scored 1-5. Each domain’s scores are calculated by adding the scores of the individual items that comprise the domain, multiplying the sum by the domain factor (sexual desire 0.6, sexual arousal and lubrication 0.3, orgasm, satisfaction, and pain 0.4). The overall score range of maternal sexual performance was 2 to 36. The cut-off point of maternal sexual dysfunction was considered less than 28. The higher scores indicated better sexual performance validity and reliability of FSFI, which have been confirmed by Rosen et al. [17]. The present study used the psychometric version in Persian [16]. In the current study, the Cronbach α coefficient was estimated as 0.87.
Each random sequence generated was recorded on a card, and the cards were placed in non-transparent, sealed, and opaque envelopes, respectively. To preserve the random sequence, the outer surface of the envelopes was numbered in the same order. Finally, the envelopes were closed and placed in a box, and participants were assigned to one of the two groups (each group 40) respectively. Farzane Karimi enrolled participants and consulted with women, Negar Asgharipour created the random sequence and allocation concealment, and Raheleh Babazadeh assigned participants to interventions.
Women in both PLISSIT and BETTER groups attended two sessions and received individual consultations weekly for two weeks in the counseling room of the given center. Each session lasted 90 minutes. The consulting time was equal for all women in 2 groups (Tables 1 and 2). FSFI was assessed at the beginning and 4 weeks after the last session.
The statistical analyst was blinded to the study. After data collection, all data were analyzed using SPSS software, version 24 (IBM, Armonk, NY, USA). The Kolmogorov-Smirnov test was used to check the normality of values. Values are expressed as Mean±SD or number (percentage). The comparison of FSFI score between ‘pre-intervention versus post-intervention’ and ‘BETTER group versus PLISSIT group’ was performed using an independent t-test and analysis of covariance. The P<0.05 was considered significant.
Results
Demographic and sexual characteristics examined and compared before the intervention and between the two study groups were homogenous in all cases. The Mean±SD ages of women were 29.7±5.5 years in the BETTER group and 31.7±5.4 years in the PLLISIT group. The majority of participants in both groups were unemployed. The kind of recent delivery in most participants in the two groups was the cesarian section (55% in BETTER and 67.5% in the PLLISIT group). The majority of participants in both groups used condoms for preventing pregnancy, 55% in BETTER and 57.5% in PLLISIT (Table 3).
The Kolmogorov-Smirnov test showed normal distribution. An independent t-test was used to compare the scores of sexual functioning at each stage between the two groups. The FSFI mean total scores in the PLLISIT and BETTER groups before the intervention were 19.5±3.6 and 18.3±4.4, respectively. However, the FSFI mean total scores in the PLLISIT and BETTER groups after the intervention were 25.1±2.0 and 25.3±1.7, respectively. The effect of the group on sexual function scores was tested using covariance analysis and score control of each variable before the intervention. The covariance analysis showed that the impact of the group on orgasm, pain, sexual desire, sexual arousal, vaginal lubrication, and FSFI total score was not statistically significant. The sexual satisfaction change after the intervention in the BETTER group was significant (P=0.015). After the intervention, the score of this domain increased by 1.4±1.0 in the PLISSIT group and 1.5±1.0 in the BETTER group (Cohen d=0.078). These results are shown in Table 4.
Discussion
The purpose of this study was to compare the effectiveness of counseling based on the standard PLISSIT and BETTER models on postpartum sexual functioning in women after childbirth.
Sexual satisfaction in the PLLISIT and BETTER groups before the intervention was not significantly different. This randomized trial showed a significant increase in sexual satisfaction in women after the intervention. In the literature, we found no study regarding women’s use of the BETTER model intervention plan in their postpartum period. The results of the present study were compared with the findings of the studies carried out via different counseling approaches and their impacts on women’s sexual function during reproductive age or after childbirth.
We found that the effect of the group on orgasm, pain, sexual desire, sexual arousal, vaginal lubrication, and FSFI total score after the intervention was not statistically significant between PLISSSIT and BETTER models. Still, sexual satisfaction in the BETTER model was increased. In another study, it was found that the BETTER model is effective in the improvement of sexual functions and sexual satisfaction in women with one to two years of infertility [18]. Another study concluded that counseling using the PLISSIT model has a positive effect on the sexual satisfaction of women [19]. One study concluded that the PLISSIT model had no significant impact on sexual function after childbirth, and using other counseling approaches was suggested [20]. One study determined the effect of counseling on sexual functioning based on the PLISSIT model on 90 postpartum breastfeeding mothers 6 months after giving birth. The study found that sexual counseling based on the PLISSIT model was effective in promoting sexual functioning compared to the control group (no intervention) [9]. Although counseling based on the PLISSIT and sexual health models was effective in the improvement of sexual function, in one study, individual therapy (PLISSIT model) was more effective than group therapy with the sexual health model [15].
Also, in this study, a comparison of the mean scores of 6 domains of sexual function in the 2 intervention groups before and 4 weeks after the intervention showed a significant difference in just one domain of sexual satisfaction. The BETTER model helps women to express their sexual life problems and prepare an appropriate treatment environment for their sexual function problems [18]. In the BETTER model, the counselor starts a dialogue, clarifies the importance of sexual issues for clients, and encourages the women to talk more about their problems. In comparison with the PLISSIT model, the counselor tries to remove the taboo of talking about sexual concerns with the husband, which can act as an impetus to self-expression and self-disclosure. Consequently, the couples begin to remove the barriers to communicating about sex that can be effective in sexual arousal and satisfaction
The results of this study show that sexual desire, orgasm, and sexual lubrication had increased and pain decreased in both groups after the intervention, but the results were not significant; these findings are in line with 2 studies that utilized the PLISSIT model in sexual education or counseling [21, 22]. This discrepancy in the pain domain may be related to cultural and personal differences in pain perception between the populations studied since culture, personal experiences, and pain tolerance deeply influence pain sensation. Lee stated that women were likely to have less sexual desire in the postpartum period due to weakness, fatigue, breastfeeding, perineal pain, reduced vaginal lubrication, and fear of wound damage or unwanted pregnancy [23].
Some studies show that although most women having resumed vaginal intercourse by 12 weeks postpartum, 30% to 62% felt pain with sex [23, 24]. The result in the domain of orgasm was in line with Mabrouk et al. [25]. The most frequent sexual disorder after 9 months postpartum included orgasm (10.8%) [26]. However, our findings disagree with the results reported by Farnam et al. [15]. The reasons for this inconsistency result from differences in study samples, questionnaires, methodologies, and psychosocial, emotional, and cognitive factors involved in women’s orgasm [27].
It should be noted that the first orgasm following childbirth can occur after 7 weeks on average (at the range of 2-18 weeks), and during the first postpartum intercourse, only 20% of women can have an orgasmic experience, which can increase to 3-6 months after childbirth [24]. In a study by Behboodi Moghadam et al., utilizing 4 sessions of sexual education program over 4 weeks could improve the sexual score of all domains of FSFI in married women with sexual dysfunction [28]. Probably more sessions are needed to increase all domains of FSFI after childbirth, and women may need more than 6 months after delivery to return to their non-pregnant condition.
One of the strengths of this study was the innovative implementation of sexual counseling based on the BETTER model for the first time after childbirth. Since the counseling sessions were conducted one-on-one, a good sample size could be considered the other strength of this study.
Among the limitations of this study was the impossibility of assessing the sexual problems of women’s marriage partners (men), so their self-reports about the absence of a sexual problem in their husbands were included in this study. The study participants were women who had actively sought help for their sexual dysfunction and, therefore, may not be representative of all postnatal women.
A comparison of the scores between the two groups of this study showed overall differences in sexual satisfaction in the BETTER group. With an emphasis on a person-centered approach and sexual communication as well as determining counseling time tailored to the client’s preferences, the BETTER sexuality model could have a greater impact on sexual functioning in clients and increase their sexual satisfaction. It can be recommended that further studies should be performed on sexual counseling after postpartum to reveal their long-term outcomes.
Ethical Considerations
Compliance with ethical guidelines
This research project was approved by the Ethics Committee of Mashhad University of Medical Sciences, Mashhad, Iran (Code: IR.MUMS.REC.1396.160) and was registered by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20170430033718N3). It was assured that the participants’ information would be kept confidential. The data were coded and anonymized on the computer. The samples were assured that they would be presented with the study results if desired.
Funding
This study was extracted from the master’s thesis of Farzaneh Karimi, approved by the Department of Midwifery, Faculty Of Nursing and Midwifery, Mashhad University of Medical Sciences. This research was supported by the Research Deputy of Mashhad University of Medical Sciences, Mashhad, Iran (Code: 951749).
Authors' contributions
Conceptualization, study design, resources, review, and editing: Farzane Karimi, Raheleh Babazadeh, Robab Latifnejad Roudsari, and Negar Asgharipour; Investigation and writing the original draft: Farzane Karimi, Raheleh Babazadeh, and Robab Latifnejad Roudsari; Data collection: Farzane Karimi and Raheleh Babazadeh; Data analysis: Habibollah Esmaeeli; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors hereby appreciate the Vice-Chancellor’s Office for Research at Mashhad University of Medical Sciences for providing financial support for this study. The authors also thank all the women who participated in this research.
References
- Niloofar H, Raheleh B, Roshanak S, Jamshid J. Evaluation of the safety and efficacy of wormwood vaginal gel in improving sexual function and sexual satisfaction in women of reproductive age: A randomized, triple-blinds, placebo-controlled clinical trial. Eur J Obstet Gynecol Reprod Biol. 2023; 280:1-6. [DOI:10.1016/j.ejogrb.2022.11.002] [PMID]
- Fuentealba-Torres M, Cartagena-Ramos D, Fronteira I, Lara LA, Arroyo LH, Arcoverde MAM, et al. What are the prevalence and factors associated with sexual dysfunction in breastfeeding women? A Brazilian cross-sectional analytical study. BMJ Open. 2019; 9(4):e025833. [DOI:10.1136/bmjopen-2018-025833] [PMID]
- McDonald E, Woolhouse H, Brown SJ. Sexual pleasure and emotional satisfaction in the first 18 months after childbirth. Midwifery. 2017; 55:60-6. [DOI:10.1016/j.midw.2017.09.002] [PMID]
- Xu XY, Yao ZW, Wang HY, Zhou Q, Zhang LW. [Women's postpartum sexuality and delivery types (Chinese)]. Zhonghua Fu Chan Ke Za Zhi. 2003; 38(4):219-22. [PMID]
- Williams A, Herron-Marx S, Carolyn H. The prevalence of enduring postnatal perineal morbidity and its relationship to perineal trauma. Midwifery. 2007; 23(4):392-403. [DOI:10.1016/j.midw.2005.12.006] [PMID]
- Karimi F, Babazadeh R, Roudsari RL, Asgharipour N, Esmaily H. Comparing the effectiveness of sexual counseling based on PLISSITand BETTER Models on sexual selfdisclosure in women with sexual problems after childbirth: A randomized trial. Iran J Nurs Midwifery Res. 2021; 26(1):68-74. [DOI:10.4103/ijnmr.IJNMR_265_19] [PMID]
- Karimi F, Babazadeh R, Asgharipour N, Esmaily H, Roudsari RL. The effectiveness of counseling using PLISSIT Model on depression, anxiety and stress, among postpartum women with sexual dysfunction: A randomized trial. J Midwifery Reprod Health. 2019; 7(4):1922-30. [DOI:10.22038/jmrh.2019.36434.1399]
- Rezaei N, Azadi A, Sayehmiri K, Valizadeh R. Postpartum sexual functioning and its predicting factors among Iranian women. Malays J Med Sci. 2017; 24(1):94-103. [DOI:10.21315/mjms2017.24.1.10] [PMID]
- Torkzahrani S, Banaei M, Ozgoli G, Azad M, Mahmoudikohani F. [The effectiveness of consultation based on plissit model on sexual function of lactating women (Persian)]. Nurs Midwifery J. 2016; 14(7):639-47. [Link]
- Taylor B, Davis S. The extended PLISSIT model for addressing the sexual wellbeing of individuals with an acquired disability or chronic illness. Sex Disabil. 2007; 25(3):135-9. [DOI:10.1007/s11195-007-9044-x]
- Quinn C, Happell B. Getting BETTER: breaking the ice and warming to the inclusion of sexuality in mental health nursing care. Int J Ment Health Nurs. 2012; 21(2):154-62. [DOI:10.1111/j.1447-0349.2011.00783.x] [PMID]
- Shalamzari KH, Asgharipour N, Jamali J, Kermani AT, Babazadeh R. The effect of sexual counseling based on BETTER and PLISSIT Model on quality of sexual life in women with breast cancer after mastectomy. J Midwifery Reprod Health. 2022; 10(4):3490-8. [Link]
- Ziaei T, Keramat A, Kharaghani R, Haseli A, Ahmadnia E. Comparing the effect of extended PLISSIT Model and group counseling on sexual function and satisfaction of pregnant women: A randomized clinical trial. J Caring Sci. 2022; 11(1):7-14. [DOI:10.34172/jcs.2022.06] [PMID]
- Hezbiiyan Z, Khodakarami B, Parsa P, Faradmal MJ. [The effect of postnatal counseling on sexual function in women referred to health centers in Hamedan in 1392 (Persian)]. Avicenna J Nurs Midwifery Care. 2016; 24(4):272-80. [DOI:10.21859/nmj-24048]
- Farnam F, Janghorbani M, Raisi F, Merghati-Khoei E. Compare the effectiveness of PLISSIT and sexual health models on women's sexual problems in Tehran, Iran: A randomized controlled trial. J Sex Med. 2014; 11(11):2679-89. [DOI:10.1111/jsm.12659] [PMID]
- Mohammadi K, Heydari M, Faghihzadeh S. [The female sexual function index (FSFI): Validation of the Iranian version (Persian)]. Payesh. 2008: 7(3):269-78. [Link]
- Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000; 26(2):191-208. [DOI:10.1080/009262300278597] [PMID]
- Karakas S, Aslan E. Sexual counseling in women with primary infertility and sexual dysfunction: Use of the BETTER Model. J Sex Marital Ther. 2019; 45(1):21-30. [DOI:10.1080/0092623X.2018.1474407] [PMID]
- Mostafa E, Ahmed AFM, Wassif GOM. Effectiveness of PLISSIT Model on Sexual Satisfaction among Newly Married Women Suffering from Sexual Problems. Paper presented at: International Congress Health Care Professionals' Innovations towards Excellence in Enhancing Quality Health Care 18th.19th October, 2017. [Link]
- Yörük F, Karaçam Z. The effectiveness of the PLISSIT Model in solving postpartum sexual problems experienced by women. Athens J Health. 2016; 3(3):235-54. [DOI:10.30958/ajh.3-3-4]
- Emam AMM, Elmenim SOA, Sabry SS. Effectiveness of application of PLISSIT counseling model on sexuality among women with dyspareunia. Am J Nurs. 2018; 7(2):73-83. [DOI:10.11648/j.ajns.20180702.15]
- Zamani M, Latifnezhad R, Moradi M, Esmaili H. [The effect of sexual counselling based on women’s postpartum sexual health program (WPSHP) on women’s sexual function and sexual quality of life (Persian). [MSc. thesis]. Mashhad: Mashhad University of Medical Sciences; 2018. Unpublished Article.
- Lee JT, Yen HW. Randomized controlled evaluation of a theory-based postpartum sexual health education programme. J Adv Nurs. 2007; 60(4):389-401. [DOI:10.1111/j.1365-2648.2007.04395.x] [PMID]
- Jawed-Wessel S, Sevick E. The impact of pregnancy and childbirth on sexual behaviors: A systematic review. J Sex Res. 2017; 54(4-5):411-23. [DOI:10.1080/00224499.2016.1274715] [PMID]
- Mabrouk M, Montanari G, Di Donato N, Del Forno S, Frascà C, Geraci E, et al. What is the impact on sexual function of laparoscopic treatment and subsequent combined oral contraceptive therapy in women with deep infiltrating endometriosis? J Sex Med. 2012; 9(3):770-8. [DOI:10.1111/j.1743-6109.2011.02593.x] [PMID]
- Banaei M, Moridi A, Dashti S. Sexual dysfunction and its associated factors after delivery: Longitudinal study in Iranian Women. Mater Sociomed. 2018; 30(3):198-203. [DOI:10.5455/msm.2018.30.198-203] [PMID]
- Mayberry L, Daniel J. 'Birthgasm': A literary review of orgasm as an alternative mode of pain relief in childbirth. J Holist Nurs. 2016; 34(4):331-42. [DOI:10.1177/0898010115614205] [PMID]
- Behboodi Moghadam Z, Rezaei E, Khaleghi Yalegonbadi F, Montazeri A, Arzaqi SM, Tavakol Z, et al. The effect of sexual health education program on women sexual function in Iran. J Res Health Sci. 2015; 15(2):124-8. [PMID]
Article Type : Research |
Subject:
Special
Received: 2021/05/5 | Accepted: 2025/05/3 | Published: 2025/06/10
Received: 2021/05/5 | Accepted: 2025/05/3 | Published: 2025/06/10
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |