Fri, Jan 30, 2026
Volume 31, Issue 2 (3-2021)
JHNM 2021, 31(2): 93-103 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hajipoor S, Pakseresht S, Niknami M, Atrkar Roshan Z, Nikandish S. The Relationship Between Social Support and Postpartum Depression. JHNM 2021; 31 (2) :93-103
URL: http://hnmj.gums.ac.ir/article-1-1600-en.html
URL: http://hnmj.gums.ac.ir/article-1-1600-en.html
Sayareh Hajipoor1 

 , Sedigheh Pakseresht *2
, Sedigheh Pakseresht *2 

 , Maryam Niknami3
, Maryam Niknami3 

 , Zahra Atrkar Roshan4
, Zahra Atrkar Roshan4 

 , Sima Nikandish5
, Sima Nikandish5 




 , Sedigheh Pakseresht *2
, Sedigheh Pakseresht *2 

 , Maryam Niknami3
, Maryam Niknami3 

 , Zahra Atrkar Roshan4
, Zahra Atrkar Roshan4 

 , Sima Nikandish5
, Sima Nikandish5 


1- Midwifery (MSc), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran
2- Professor, Social Determinants of Health Research Center (SDHRC), Reproductive Health Research Center, Department of Obstetrics, Women Health Promotion, Community Health, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran ,nmjpakseresht@gmail.com
3- Instructor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran
4- Associate Professor, Department of Bio-Statistics, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
5- Midwifery (MSc), Zanjan University of medical sciences, Zanjan, Iran
2- Professor, Social Determinants of Health Research Center (SDHRC), Reproductive Health Research Center, Department of Obstetrics, Women Health Promotion, Community Health, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran ,
3- Instructor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran
4- Associate Professor, Department of Bio-Statistics, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
5- Midwifery (MSc), Zanjan University of medical sciences, Zanjan, Iran
Full-Text [PDF 557 kb]
(1236 Downloads)
| Abstract (HTML) (2759 Views)
Full-Text: (2379 Views)
Introduction
regnancy, childbirth, and adapting to the new circumstances of a newborn baby in the family can be considered the most critical stage of a woman’s life development [1, 2]. Pregnancy and postpartum are essential times for mothers and their families [3], and those who are experiencing this stage for the first time need more support during this period [4]. In this period, the mothers endure changes in physical, psychological, economic, and social systems [5], physical care of the baby, attention to growth and development [6, 7], sucking and breastfeeding problems, jaundice, sleep disturbance, baby weight gain, bloating, eye infections and the umbilical cord [8] headache, back pain, urinary incontinence and the feeling of physical exhaustion [9, 10, 11]. The postpartum period is when the mother is confronted with newer roles, patterns, and relationships and is more prone than ever to emotional and mood crises, including depression [12]. This period, as a stage of change in the mother’s life, needs readjusting [3].
Depression is the most common postpartum psychological problem that affects the health of mother and baby [4, 13, 14]. Depression is associated with decreased mood and loss of interest, guilt, worthlessness, sleep and appetite disorders, decreased energy, and weakness [15], which can lead to impaired and inability to care for the baby, increase the risk of neonatal homicide and suicide [16, 17, 18]. Significant symptoms of postpartum depression include sleep disturbance, lack of concentration, low self-esteem, deep sadness and frequent cries, feelings of hopelessness and loneliness, feelings of doubt, and suicidal thoughts [4, 18]. The prevalence of depression, especially postpartum depression, is closely related to cultural and social factors, and therefore its frequency in countries and different races are different [1]. The prevalence of postpartum depression in the world is estimated at 10%-15% [19]. In Iran studies, the prevalence of postpartum depression has been reported up to 43.5% [20, 21].
One of the factors that may be associated with postpartum depression is social support [22]. Social support refers to the amount of respect, sense of belonging, love, and affection that a person receives from others [22, 23]. Social support can have a positive interaction with mother self-efficacy and mother-infant attachment [24, 25]. Studies have shown that people who receive adequate social support can adapt better to problems and have a good psychological adjustment [23, 26].
The results of some studies confirm that receiving support from spause, family and friends have a significant relationship with reducing postpartum depression [4, 13, 19]. The impact of this support has been reported in different races and cultures [13]. Social support plays an essential role in maintaining the psychological health of mothers and infants and the lack of social support is a significant risk factor for postpartum depression [2]. Strong social bonds act as a protection or barrier against depression during pregnancy and delivery [2, 27]. So, this study was conducted to determine the relationship between social support and postpartum depression.
Materials and Methods
The present study is a cross-sectional analytical study of correlation type performed on 300 mothers referred to the comprehensive health centers of Guilan University of Medical Sciences in Rasht City, Iran, 2 to 4 weeks after their deliveries.
The inclusion criteria include full-term pregnancy, singleton, no underlying disease and history of depression in previous pregnancies (based on the self-report), low-risk pregnancy (history of heart disease, diabetes, hypertension, thyroid, etc.), having a healthy baby, no history of hospitalization during the current pregnancy, no recent difficult delivery, no addiction, no use of psychiatric medications before and during the recent pregnancy, and no encounter with unpleasant and stressful events in the last year (such as first-degree death).
The sampling was done by cluster sampling method selected from 20 comprehensive health service centers and 41 bases in the north, south, east, and west and the center of Rasht City, Iran. Out of these centers, 20 clusters were selected by systematic random method. Since the number of people covered by the comprehensive health service centers was almost equal, the number of samples was selected equally from each group of 15 people for 5 months (from July to October 2018). The required sample size was obtained 300, based on a preliminary study on 20 mothers with the characteristics of the studied units and the relationship between postpartum depression and social support (r=0.2) with a 95% confidence, 80% test power, and 10% drop of samples.
The study data were collected using a three-part questionnaire and through interviews with samples. The first part of the maternal and infant demographic questionnaire included mother’s age, mother’s education, occupation, spause’s occupation, income, place of residence, residence status, number of deliveries, number of abortions and stillbirths, sex of the baby, type of delivery, birth weight, number of pregnancy care and type of pregnancy.
The second part consisted of the standard Hopkins social support questionnaire [28], which measures the amount of social support after childbirth with 44 items. This questionnaire was designed by Hopkins (2008) and had 4 domains: social support from the partner (spause) (items 1-13), mother’s parents (items 14-23), spause’s parents (items 24-31), friends and relatives (items 32–44) and is scored on a 5-point Likert scale from never=0, rarely=1, sometimes=2, most of the time=3, and always=4. Besides, items 6, 8, 9 have inverse scoring. The total score of the questionnaire is between 0 and 176. Higher scores indicate more social support. Matching scores in different domains of spause, parents, spauses’ parents, friends, and relatives have been balanced and reported from 0 to 100. To determine the scientific validity of the social support questionnaire, the content validity method was used, and its Persian version was provided to 10 faculty members of related fields. Accordingly, the CVR (content validity ratio) was more than 0.62, and the CVI (content validity index) was more than 79%. To determine the internal consistency of the instrument, a preliminary study was performed on 20 individuals with the inclusion criteria, and the internal consistency was confirmed by determining the alpha coefficient (α=0.78).
The Edinburgh Postpartum Depression Scale (EPDS) questionnaire was designed in 2006. Ahmadi Kani assessed its psychometrics in Iran [16]. The questionnaire consists of 10 questions that allow the diagnosis of depression within 2 to 4 weeks after delivery, and its score ranges between 0 and 30, and a score of 12 or more is considered as postpartum depression. Also, the score was divided between 0-10 (mild), 10 -20 (moderate), and 20-30 (severe). Questions 4, 2, 1 are scored from 0 to 3, and questions 10, 9, 8, 7, 6, 5, 3 are scored from the Likert scale of 3 to 0.
The social support score did not follow the normal distribution in general according to the Komolo Smirnov and Shapiro-Wilk tests. To analyze the data, descriptive statistics indicators and Friedman, Mann-Whitney U, Kruskal-Wallis tests, the Spearman correlation coefficient, and logistic regression model were used and conducted in SPSS version 21. A P value of less than 0.05 was considered significant.
Results
The results showed that the mean±SD age of mothers was 29±5.3 years, birth weight was 3346±408.68 g and the frequency of receiving antenatal care was 7.7±2.7 times. Other personal and social characteristics of the samples are presented in Table 1.
.jpg)
Comparing the statistical indicators of adjusted scores of social support in general and separate domains, the results showed that according to the Friedman test, the scores of different domains of social support have a statistically significant difference (P=0.001), which is the highest social support score was on the part of the spause with a mean of 77.96±14.98, and the lowest was related to the friends and relatives with an average of 48.5±24.8. In general, the mean±SD social support score in the samples was 64.03±16.9 (Table 2).
.jpg)
The results showed that the status of postpartum depression symptoms in this study was 67.3% mild and only 11% severe (Figure 1). Between the score of depression and the score of social support from the spause (P=0.004, r=-0.167), parents (P=0.002, r=-0.176), and the score of total social support (P=0.024, r=-0.130), there was a significant inverse correlation. Still, the relationships between the spause’s parents, friends, and relatives were not significant (Table 3).
.jpg)
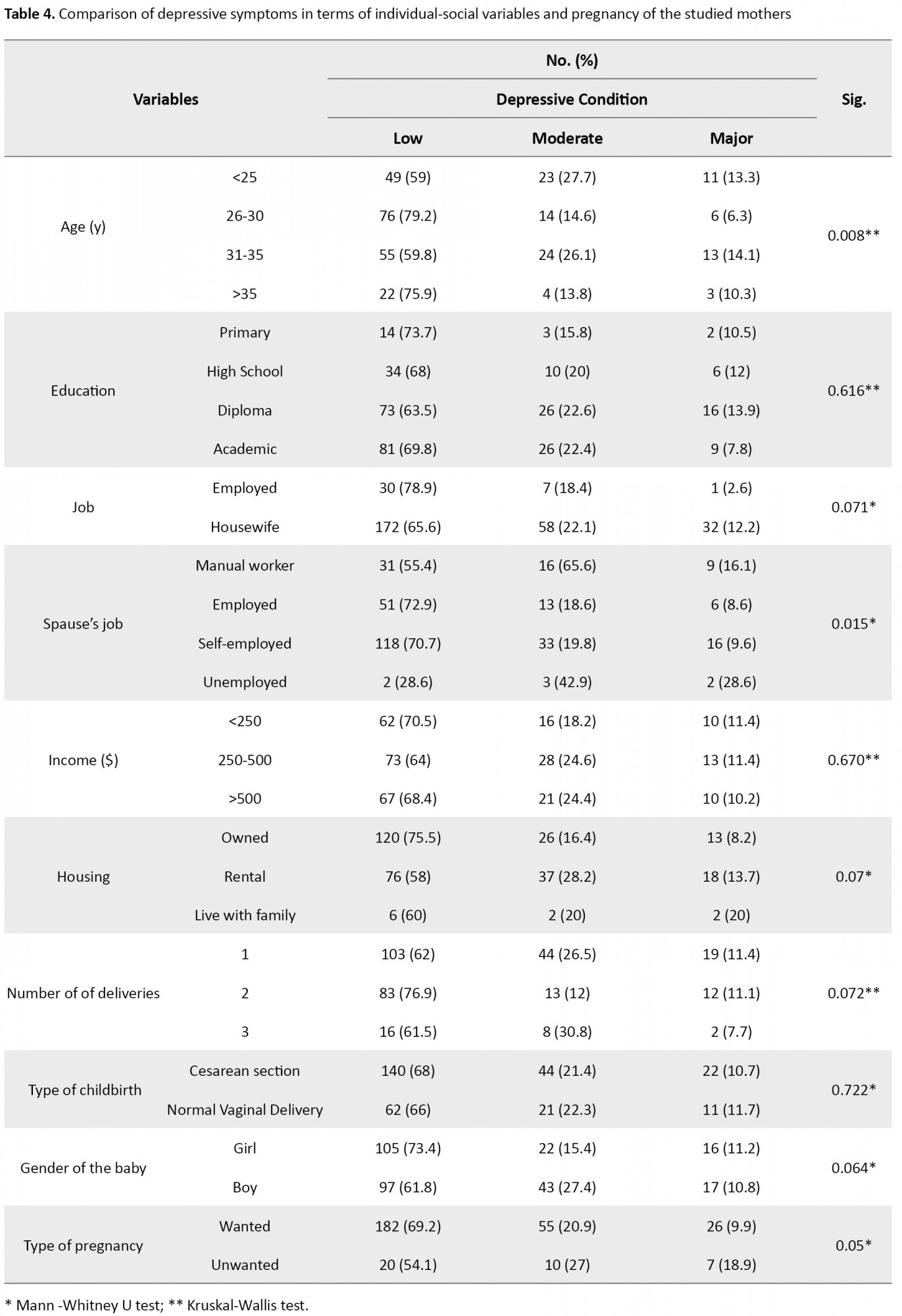
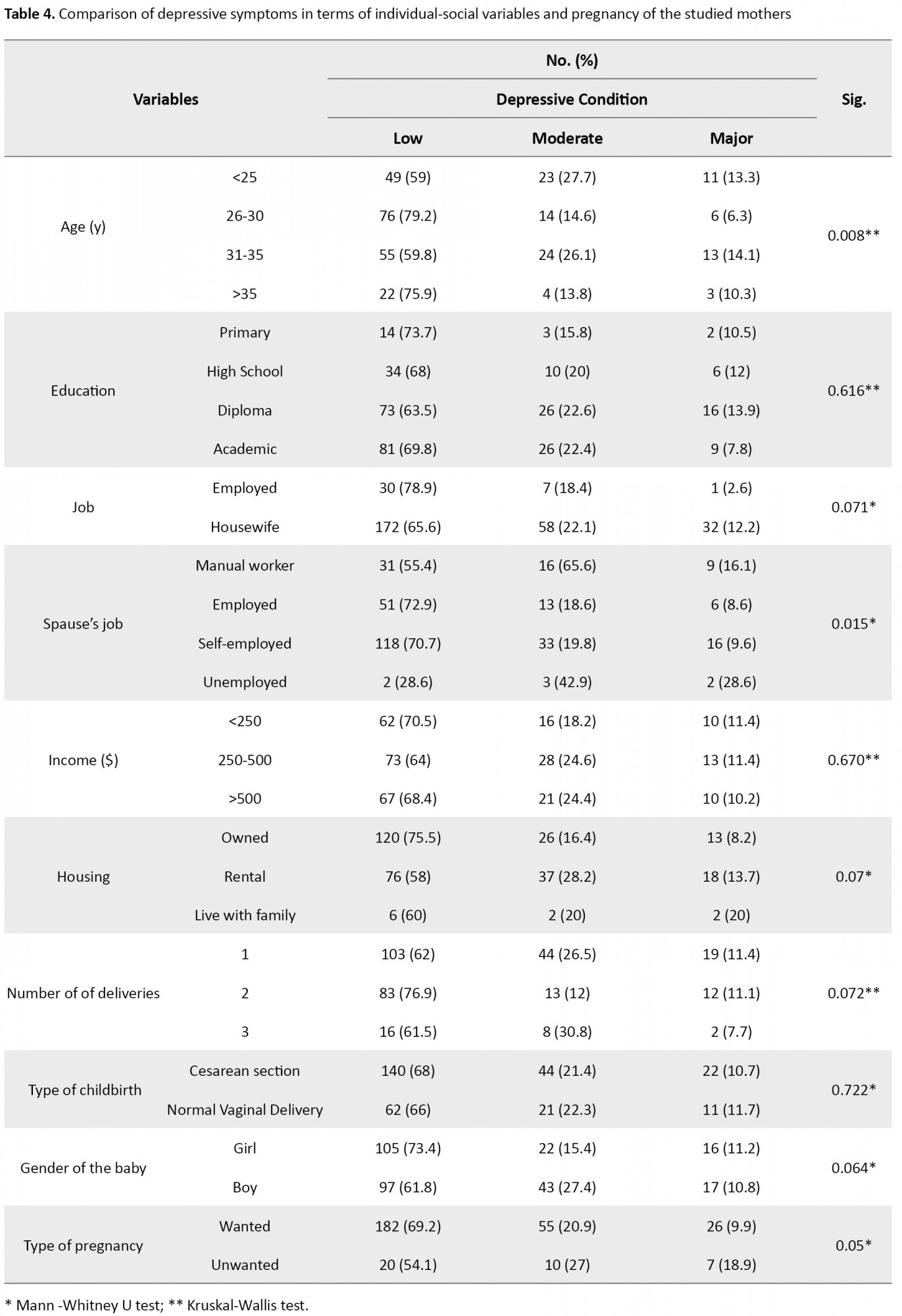
The results also showed that the depressive status in terms of age (P=0.008), spause’s occupation (P=0.015), and type of pregnancy (P=0.05) had a statistically significant difference (Table 4).
In addition, the results showed that the relationship between social support score and income (P=0.001, r=0.292) and the number of deliveries (P=0.022, r=-0.132) was statistically significant.
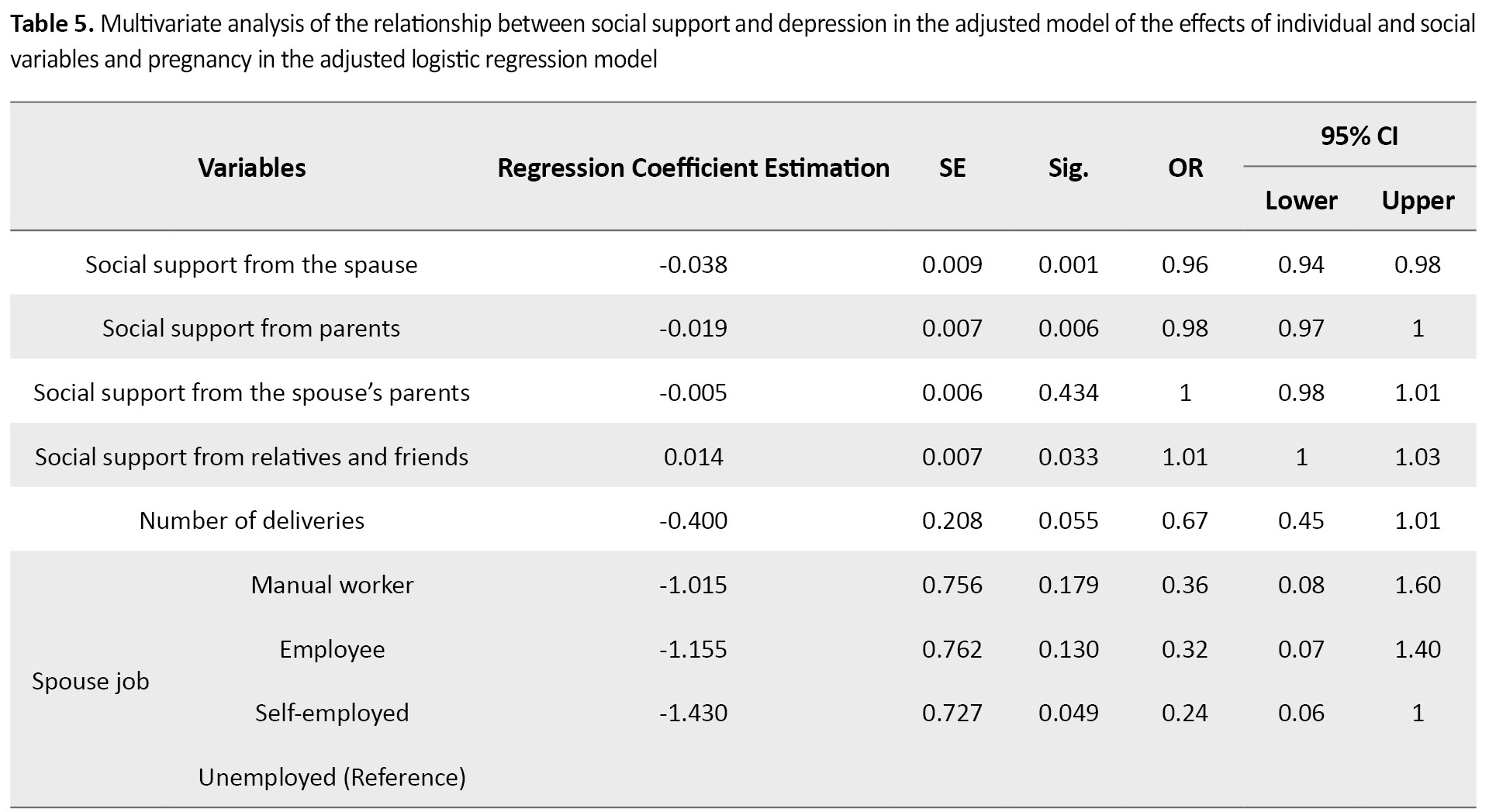
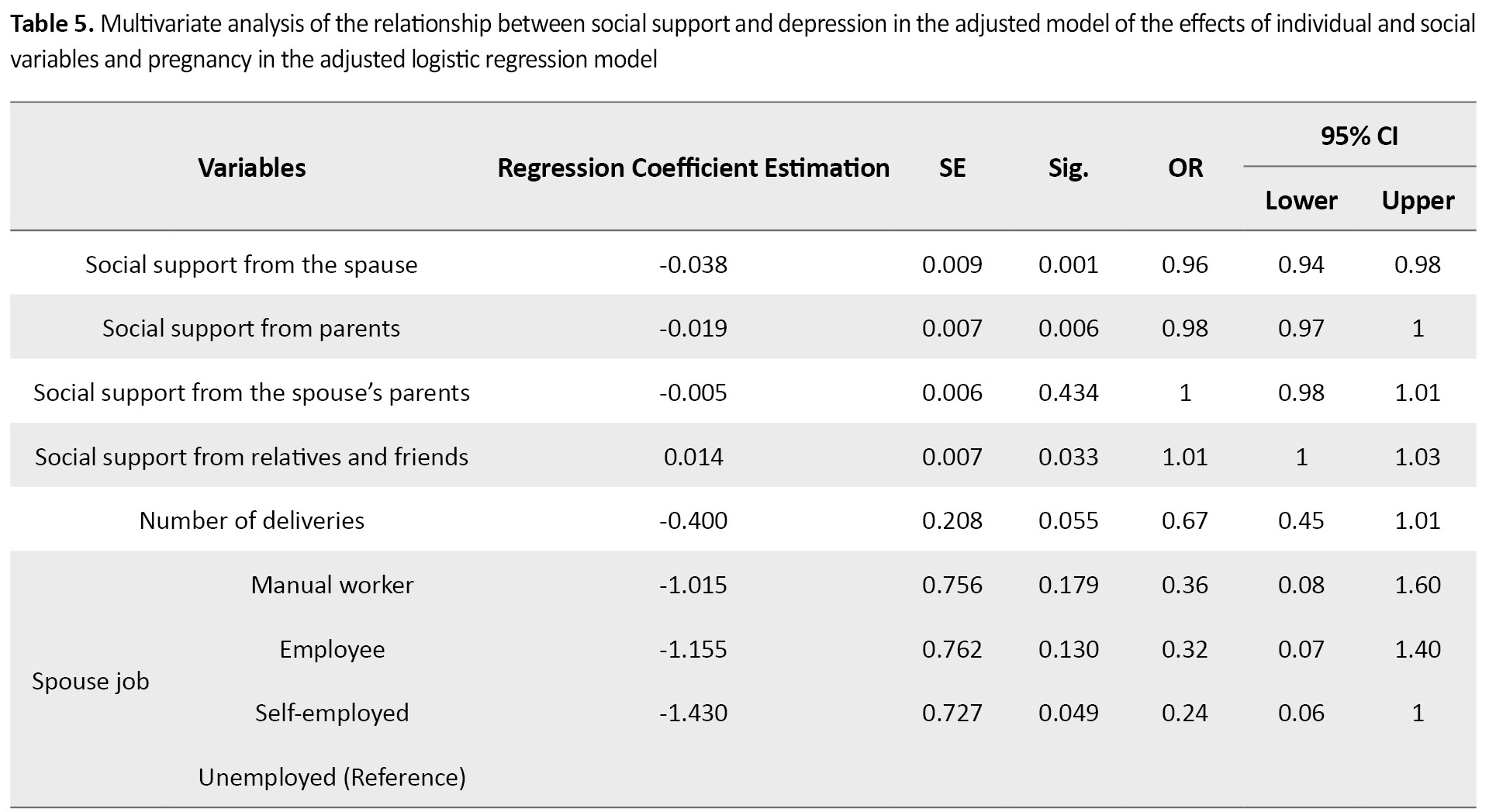
Multiple analysis of the correlation between the scores of social support areas and depression using the logistic regression model of rank by modulating the effects of individual social and pregnancy variables (adjusted model) showed the score of social support by the spause (OR=0.96, CI: 0.94-0.98, P=0.001), parents (OR=0.98, CI; 0.97-1, P=0.006), friends and relatives (OR=1.01, CI; 1-1.03, P=0.033) were associated with the severity of depression, as well as the number of deliveries (OR=0.67, CI; 0.45-1.01, P=0.005) and the occupation of spauses (self-employed) versus the unemployed (OR=0.24, CI; 0.06-1, P=0.049) have been predictors of postpartum depression (Table 5).
Discussion
The results of the present study showed that the prevalence of postpartum depression symptoms was mild in most of the studied units. However, Ghaljeh reported the prevalence of postpartum depression in a study in Najafabad, Isfahan Province, Iran, as mild in only one-third of the samples [29]. The observed differences can be due to the variation in the prevalence of postpartum depression in different cultures and races, indicating its relationship with cultural and social factors. It may also be due to differences in the tools used and measuring time of depression and the most importantly, because of differences in the research communities.
The results of the present study also showed that the mean±SD total score of social support was 64.03±16.9. The mean±SD total score of social support was reported 69.3±9 by Nago [30], 64.63±8.13 (6 weeks after delivery) by Gao [31], and 66.4±9.1 (4 weeks postpartum) by Li [32]. The tools used by these researchers were similar to the tools used in this study. Nazari [33] reported the mean±SD total score of social support as 96±24.7 (4 weeks after delivery), and Shafiee [34] reported 92.02±21.49. In the present study, mothers participated who delivered their first to third children, while in the theoretical research community, only multiparous mothers participated. In the Shafiee study, the mothers with premature infants participated. Or perhaps because social support is a multidimensional concept, the results may also be influenced by the environment in which the information was collected.
During pregnancy and the first few weeks after childbirth, support for mothers in Iran is traditionally high by their relatives. But in general, and after 40 days post-delivery, mothers and children are faced with the new world alone, a situation that is less noticeable in multi-para mothers because people think that they already have experience more than in primiparous mothers [34]. Hung also reported that the level of social support decreases from the first to the sixth week after delivery [9]. The similarity of the results of the Gao study may also be due to the traditional Chinese culture, as in Eastern societies, women have a significant and high position in the family, and the majority of families with different situations and cultures support women during pregnancy and postpartum [31]. Also, supporting the wife creates self-esteem, respect, and safety during pregnancy and postpartum [35].
Another result of the present study is comparing the total social support score in terms of personal-social with pregnancy variables in mothers regarding educational level, job, spause’s job, income, residence status, number of deliveries, and pregnancy type. In Shafiee study, there was no statistically significant relationship between education level, mother’s job, and social support, while they reported a significant relationship between social support and spause’s job, number of deliveries, and family economic status [34], which the present study consistent with it. The results of the Cheng study in the United States showed a significant relationship between social support and the number of deliveries and employment [36]. In Bakhtiyari study, social support was not significantly related to education and employment [26]. Vaezi also did not report a significant relationship between social support with education level, employment, and pregnancy type [19], which the present study is not consistent with them. Saberi also reported that social support was unrelated to residence status [22], which is inconsistent with the current study result. This difference may be related to the culture of the research community and the research tools. Shafiee [34] and Azimi [35], in their study, also reported a significant relationship between social support and income that the present study is consistent with their results.
There was a statistically significant relationship between depressive status and age, spause’s occupation, and type of pregnancy. As mothers within an age range of 26-30 years and with the occupation of spauses (employee) and type of pregnancy (wanted) had the lowest rate of depression. Strelow in the United States, on the other hand, has shown that younger mothers, aged 15-24 years (compared to older mothers of 25-29 years), are less prone to depression [37]. Guin [38] also stated that mothers within an age range of 36-40 years reported the highest rate of depression, and those within a range of 20-25 years had the lowest. Differences in the results may be due to unwanted pregnancy or lack of family support, which has increased the chances of postpartum depression.
There is also a significant inverse correlation between postpartum depression and social support from the spause and the parents. Shafiee’s study [34], reported that social support could be effective in increasing the mental health of mothers, and its ignorance by the family, life partner, and mother had the greatest impact on maternal depression, which is in line.
The results of the present study, after adjusting the personal, social, and fertility variables in women, a relationship was found between social support from spause, parents (inverse), friends, and relatives (direct) and the severity of depression. Noury [23] also showed a negative correlation between depression and social support; however, mothers who receive higher social support from friends and family experienced less postpartum depression. This relationship was significant with the number of deliveries and the spauses’ occupation (self-employed versus the unemployed). Shafiee [34] also concluded a statistically significant relationship between social support and the spouse’s job because social support is defined as the amount of love, companionship, and attention of family members, friends, and others. Awareness of the sources of support causes people to believe that they have the help of others to change a situation or event [15].
One of the limitations of this study is the self-report of mothers who may, in some cases, have refused to state the facts. It has also been a one-step study and failed to review the continuity of social support. This study was performed on urban mothers referring to comprehensive health service centers in Rasht City. Due to the cultural factor, rural mothers may experience different environmental stresses after giving birth. The rate of postpartum depression in them may also be different. Therefore, it is suggested that a similar comparative study be performed in rural and urban mothers.
The results of the present study showed that the amount of social support decreases with increasing the number of deliveries and unwanted pregnancies. Also, the amount of social support among friends and acquaintances was less than the other three areas. Therefore, due to the aging population in the country and the need to increase the population growth rate with on-time childbirth, it is necessary to improve social support for this vulnerable group with the help of the Ministry of health. Also, these measures should be guided and supported by family members, relatives, spauses, friends, midwives, and comprehensive health centers. Therefore, education to the family and support of mothers in these four areas (spause, wife’s parents, spause parents, and friends and relatives) are recommended. Obviously, postpartum depression will decline by increasing the social support.
Therefore, midwives should be in close contact with mothers in hospitals and comprehensive health service centers, in informing about the symptoms of postpartum depression and screening before or during pregnancy and after delivery and even educating health liaisons and health workers (in the first level of prevention) who are responsible for health education and care at this level. They can identify vulnerable mothers and refer them to doctors and take action to prevent them at higher levels.
Also, media can raise the culture of not stigmatizing depressed mothers and informing people in the community (especially family members, friends, and relatives) that postpartum depression can be treated like other diseases such as diabetes and high blood pressure, and so on. Failure to treat in time may lead to more complications, so it is necessary to consider postpartum depression a normal outcome and encourage mothers to seek treatment.
Ethical Considerations
Compliance with ethical guidelines
Ethical permission was obtained from the Research Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.2018.121 on 2/4/2018).
Funding
This research was funded by the Master Research Project from Guilan University of Medical Sciences and Social Determinants of Health Research Center (SDHRC).
Authors contributions
Concept: Sedigheh Pakseresht, Sayareh Hajipoor, Marayam Niknami, Zahra Atrkar Roushan; Writing the original draft: Sedigheh Pakseresht, Sayareh Hajipoor, Marayam Niknami , Zahra Atrkar Roushan and Sima Nikandish; Data collection: Sayareh Hajipoor; Data analysis: Sedigheh Pakseresht, Sayareh Hajipoor, Marayam Niknami, Zahra Atrkar Roushan, Sima Nikandish; Reviewing the final edition: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We would like to thank all mothers who participated in this study and all people who helped us.
References
regnancy, childbirth, and adapting to the new circumstances of a newborn baby in the family can be considered the most critical stage of a woman’s life development [1, 2]. Pregnancy and postpartum are essential times for mothers and their families [3], and those who are experiencing this stage for the first time need more support during this period [4]. In this period, the mothers endure changes in physical, psychological, economic, and social systems [5], physical care of the baby, attention to growth and development [6, 7], sucking and breastfeeding problems, jaundice, sleep disturbance, baby weight gain, bloating, eye infections and the umbilical cord [8] headache, back pain, urinary incontinence and the feeling of physical exhaustion [9, 10, 11]. The postpartum period is when the mother is confronted with newer roles, patterns, and relationships and is more prone than ever to emotional and mood crises, including depression [12]. This period, as a stage of change in the mother’s life, needs readjusting [3].
Depression is the most common postpartum psychological problem that affects the health of mother and baby [4, 13, 14]. Depression is associated with decreased mood and loss of interest, guilt, worthlessness, sleep and appetite disorders, decreased energy, and weakness [15], which can lead to impaired and inability to care for the baby, increase the risk of neonatal homicide and suicide [16, 17, 18]. Significant symptoms of postpartum depression include sleep disturbance, lack of concentration, low self-esteem, deep sadness and frequent cries, feelings of hopelessness and loneliness, feelings of doubt, and suicidal thoughts [4, 18]. The prevalence of depression, especially postpartum depression, is closely related to cultural and social factors, and therefore its frequency in countries and different races are different [1]. The prevalence of postpartum depression in the world is estimated at 10%-15% [19]. In Iran studies, the prevalence of postpartum depression has been reported up to 43.5% [20, 21].
One of the factors that may be associated with postpartum depression is social support [22]. Social support refers to the amount of respect, sense of belonging, love, and affection that a person receives from others [22, 23]. Social support can have a positive interaction with mother self-efficacy and mother-infant attachment [24, 25]. Studies have shown that people who receive adequate social support can adapt better to problems and have a good psychological adjustment [23, 26].
The results of some studies confirm that receiving support from spause, family and friends have a significant relationship with reducing postpartum depression [4, 13, 19]. The impact of this support has been reported in different races and cultures [13]. Social support plays an essential role in maintaining the psychological health of mothers and infants and the lack of social support is a significant risk factor for postpartum depression [2]. Strong social bonds act as a protection or barrier against depression during pregnancy and delivery [2, 27]. So, this study was conducted to determine the relationship between social support and postpartum depression.
Materials and Methods
The present study is a cross-sectional analytical study of correlation type performed on 300 mothers referred to the comprehensive health centers of Guilan University of Medical Sciences in Rasht City, Iran, 2 to 4 weeks after their deliveries.
The inclusion criteria include full-term pregnancy, singleton, no underlying disease and history of depression in previous pregnancies (based on the self-report), low-risk pregnancy (history of heart disease, diabetes, hypertension, thyroid, etc.), having a healthy baby, no history of hospitalization during the current pregnancy, no recent difficult delivery, no addiction, no use of psychiatric medications before and during the recent pregnancy, and no encounter with unpleasant and stressful events in the last year (such as first-degree death).
The sampling was done by cluster sampling method selected from 20 comprehensive health service centers and 41 bases in the north, south, east, and west and the center of Rasht City, Iran. Out of these centers, 20 clusters were selected by systematic random method. Since the number of people covered by the comprehensive health service centers was almost equal, the number of samples was selected equally from each group of 15 people for 5 months (from July to October 2018). The required sample size was obtained 300, based on a preliminary study on 20 mothers with the characteristics of the studied units and the relationship between postpartum depression and social support (r=0.2) with a 95% confidence, 80% test power, and 10% drop of samples.
The study data were collected using a three-part questionnaire and through interviews with samples. The first part of the maternal and infant demographic questionnaire included mother’s age, mother’s education, occupation, spause’s occupation, income, place of residence, residence status, number of deliveries, number of abortions and stillbirths, sex of the baby, type of delivery, birth weight, number of pregnancy care and type of pregnancy.
The second part consisted of the standard Hopkins social support questionnaire [28], which measures the amount of social support after childbirth with 44 items. This questionnaire was designed by Hopkins (2008) and had 4 domains: social support from the partner (spause) (items 1-13), mother’s parents (items 14-23), spause’s parents (items 24-31), friends and relatives (items 32–44) and is scored on a 5-point Likert scale from never=0, rarely=1, sometimes=2, most of the time=3, and always=4. Besides, items 6, 8, 9 have inverse scoring. The total score of the questionnaire is between 0 and 176. Higher scores indicate more social support. Matching scores in different domains of spause, parents, spauses’ parents, friends, and relatives have been balanced and reported from 0 to 100. To determine the scientific validity of the social support questionnaire, the content validity method was used, and its Persian version was provided to 10 faculty members of related fields. Accordingly, the CVR (content validity ratio) was more than 0.62, and the CVI (content validity index) was more than 79%. To determine the internal consistency of the instrument, a preliminary study was performed on 20 individuals with the inclusion criteria, and the internal consistency was confirmed by determining the alpha coefficient (α=0.78).
The Edinburgh Postpartum Depression Scale (EPDS) questionnaire was designed in 2006. Ahmadi Kani assessed its psychometrics in Iran [16]. The questionnaire consists of 10 questions that allow the diagnosis of depression within 2 to 4 weeks after delivery, and its score ranges between 0 and 30, and a score of 12 or more is considered as postpartum depression. Also, the score was divided between 0-10 (mild), 10 -20 (moderate), and 20-30 (severe). Questions 4, 2, 1 are scored from 0 to 3, and questions 10, 9, 8, 7, 6, 5, 3 are scored from the Likert scale of 3 to 0.
The social support score did not follow the normal distribution in general according to the Komolo Smirnov and Shapiro-Wilk tests. To analyze the data, descriptive statistics indicators and Friedman, Mann-Whitney U, Kruskal-Wallis tests, the Spearman correlation coefficient, and logistic regression model were used and conducted in SPSS version 21. A P value of less than 0.05 was considered significant.
Results
The results showed that the mean±SD age of mothers was 29±5.3 years, birth weight was 3346±408.68 g and the frequency of receiving antenatal care was 7.7±2.7 times. Other personal and social characteristics of the samples are presented in Table 1.
.jpg)
Comparing the statistical indicators of adjusted scores of social support in general and separate domains, the results showed that according to the Friedman test, the scores of different domains of social support have a statistically significant difference (P=0.001), which is the highest social support score was on the part of the spause with a mean of 77.96±14.98, and the lowest was related to the friends and relatives with an average of 48.5±24.8. In general, the mean±SD social support score in the samples was 64.03±16.9 (Table 2).
.jpg)
The results showed that the status of postpartum depression symptoms in this study was 67.3% mild and only 11% severe (Figure 1). Between the score of depression and the score of social support from the spause (P=0.004, r=-0.167), parents (P=0.002, r=-0.176), and the score of total social support (P=0.024, r=-0.130), there was a significant inverse correlation. Still, the relationships between the spause’s parents, friends, and relatives were not significant (Table 3).
.jpg)
The results also showed that the depressive status in terms of age (P=0.008), spause’s occupation (P=0.015), and type of pregnancy (P=0.05) had a statistically significant difference (Table 4).
In addition, the results showed that the relationship between social support score and income (P=0.001, r=0.292) and the number of deliveries (P=0.022, r=-0.132) was statistically significant.
Multiple analysis of the correlation between the scores of social support areas and depression using the logistic regression model of rank by modulating the effects of individual social and pregnancy variables (adjusted model) showed the score of social support by the spause (OR=0.96, CI: 0.94-0.98, P=0.001), parents (OR=0.98, CI; 0.97-1, P=0.006), friends and relatives (OR=1.01, CI; 1-1.03, P=0.033) were associated with the severity of depression, as well as the number of deliveries (OR=0.67, CI; 0.45-1.01, P=0.005) and the occupation of spauses (self-employed) versus the unemployed (OR=0.24, CI; 0.06-1, P=0.049) have been predictors of postpartum depression (Table 5).
Discussion
The results of the present study showed that the prevalence of postpartum depression symptoms was mild in most of the studied units. However, Ghaljeh reported the prevalence of postpartum depression in a study in Najafabad, Isfahan Province, Iran, as mild in only one-third of the samples [29]. The observed differences can be due to the variation in the prevalence of postpartum depression in different cultures and races, indicating its relationship with cultural and social factors. It may also be due to differences in the tools used and measuring time of depression and the most importantly, because of differences in the research communities.
The results of the present study also showed that the mean±SD total score of social support was 64.03±16.9. The mean±SD total score of social support was reported 69.3±9 by Nago [30], 64.63±8.13 (6 weeks after delivery) by Gao [31], and 66.4±9.1 (4 weeks postpartum) by Li [32]. The tools used by these researchers were similar to the tools used in this study. Nazari [33] reported the mean±SD total score of social support as 96±24.7 (4 weeks after delivery), and Shafiee [34] reported 92.02±21.49. In the present study, mothers participated who delivered their first to third children, while in the theoretical research community, only multiparous mothers participated. In the Shafiee study, the mothers with premature infants participated. Or perhaps because social support is a multidimensional concept, the results may also be influenced by the environment in which the information was collected.
During pregnancy and the first few weeks after childbirth, support for mothers in Iran is traditionally high by their relatives. But in general, and after 40 days post-delivery, mothers and children are faced with the new world alone, a situation that is less noticeable in multi-para mothers because people think that they already have experience more than in primiparous mothers [34]. Hung also reported that the level of social support decreases from the first to the sixth week after delivery [9]. The similarity of the results of the Gao study may also be due to the traditional Chinese culture, as in Eastern societies, women have a significant and high position in the family, and the majority of families with different situations and cultures support women during pregnancy and postpartum [31]. Also, supporting the wife creates self-esteem, respect, and safety during pregnancy and postpartum [35].
Another result of the present study is comparing the total social support score in terms of personal-social with pregnancy variables in mothers regarding educational level, job, spause’s job, income, residence status, number of deliveries, and pregnancy type. In Shafiee study, there was no statistically significant relationship between education level, mother’s job, and social support, while they reported a significant relationship between social support and spause’s job, number of deliveries, and family economic status [34], which the present study consistent with it. The results of the Cheng study in the United States showed a significant relationship between social support and the number of deliveries and employment [36]. In Bakhtiyari study, social support was not significantly related to education and employment [26]. Vaezi also did not report a significant relationship between social support with education level, employment, and pregnancy type [19], which the present study is not consistent with them. Saberi also reported that social support was unrelated to residence status [22], which is inconsistent with the current study result. This difference may be related to the culture of the research community and the research tools. Shafiee [34] and Azimi [35], in their study, also reported a significant relationship between social support and income that the present study is consistent with their results.
There was a statistically significant relationship between depressive status and age, spause’s occupation, and type of pregnancy. As mothers within an age range of 26-30 years and with the occupation of spauses (employee) and type of pregnancy (wanted) had the lowest rate of depression. Strelow in the United States, on the other hand, has shown that younger mothers, aged 15-24 years (compared to older mothers of 25-29 years), are less prone to depression [37]. Guin [38] also stated that mothers within an age range of 36-40 years reported the highest rate of depression, and those within a range of 20-25 years had the lowest. Differences in the results may be due to unwanted pregnancy or lack of family support, which has increased the chances of postpartum depression.
There is also a significant inverse correlation between postpartum depression and social support from the spause and the parents. Shafiee’s study [34], reported that social support could be effective in increasing the mental health of mothers, and its ignorance by the family, life partner, and mother had the greatest impact on maternal depression, which is in line.
The results of the present study, after adjusting the personal, social, and fertility variables in women, a relationship was found between social support from spause, parents (inverse), friends, and relatives (direct) and the severity of depression. Noury [23] also showed a negative correlation between depression and social support; however, mothers who receive higher social support from friends and family experienced less postpartum depression. This relationship was significant with the number of deliveries and the spauses’ occupation (self-employed versus the unemployed). Shafiee [34] also concluded a statistically significant relationship between social support and the spouse’s job because social support is defined as the amount of love, companionship, and attention of family members, friends, and others. Awareness of the sources of support causes people to believe that they have the help of others to change a situation or event [15].
One of the limitations of this study is the self-report of mothers who may, in some cases, have refused to state the facts. It has also been a one-step study and failed to review the continuity of social support. This study was performed on urban mothers referring to comprehensive health service centers in Rasht City. Due to the cultural factor, rural mothers may experience different environmental stresses after giving birth. The rate of postpartum depression in them may also be different. Therefore, it is suggested that a similar comparative study be performed in rural and urban mothers.
The results of the present study showed that the amount of social support decreases with increasing the number of deliveries and unwanted pregnancies. Also, the amount of social support among friends and acquaintances was less than the other three areas. Therefore, due to the aging population in the country and the need to increase the population growth rate with on-time childbirth, it is necessary to improve social support for this vulnerable group with the help of the Ministry of health. Also, these measures should be guided and supported by family members, relatives, spauses, friends, midwives, and comprehensive health centers. Therefore, education to the family and support of mothers in these four areas (spause, wife’s parents, spause parents, and friends and relatives) are recommended. Obviously, postpartum depression will decline by increasing the social support.
Therefore, midwives should be in close contact with mothers in hospitals and comprehensive health service centers, in informing about the symptoms of postpartum depression and screening before or during pregnancy and after delivery and even educating health liaisons and health workers (in the first level of prevention) who are responsible for health education and care at this level. They can identify vulnerable mothers and refer them to doctors and take action to prevent them at higher levels.
Also, media can raise the culture of not stigmatizing depressed mothers and informing people in the community (especially family members, friends, and relatives) that postpartum depression can be treated like other diseases such as diabetes and high blood pressure, and so on. Failure to treat in time may lead to more complications, so it is necessary to consider postpartum depression a normal outcome and encourage mothers to seek treatment.
Ethical Considerations
Compliance with ethical guidelines
Ethical permission was obtained from the Research Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.2018.121 on 2/4/2018).
Funding
This research was funded by the Master Research Project from Guilan University of Medical Sciences and Social Determinants of Health Research Center (SDHRC).
Authors contributions
Concept: Sedigheh Pakseresht, Sayareh Hajipoor, Marayam Niknami, Zahra Atrkar Roushan; Writing the original draft: Sedigheh Pakseresht, Sayareh Hajipoor, Marayam Niknami , Zahra Atrkar Roushan and Sima Nikandish; Data collection: Sayareh Hajipoor; Data analysis: Sedigheh Pakseresht, Sayareh Hajipoor, Marayam Niknami, Zahra Atrkar Roushan, Sima Nikandish; Reviewing the final edition: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We would like to thank all mothers who participated in this study and all people who helped us.
References
- Rahmani F, Seyedfatemi N, Asadollahi M, Seyedrasooli A. [Predisposing factors of postpartum depression (Persian)]. Iran Journal of Nursing. 2011; 24(72):78-87. http://ijn.iums.ac.ir/article-1-1032-en.html
- Pourkhaleghi N, Askarizadeh Gh, Fazilatpour M. [Predicting post-partum depression of nulliparous women: Role of social support and delivery type (Persian)]. Journal of Health & Care. 2017; 19(1):18-29. http://hcjournal.arums.ac.ir/article-1-701-en.html
- Alipour Z, Lamyian M, Hajizadeh E. [Sleep quality in late pregnancy and postpartum depression (Persian)]. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2012; 14(8):39-47. [DOI:10.22038/IJOGI.2012.6002]
- Tambag H, Turan Z, Tolun S, Can R. Perceived social support and depression levels of women in the postpartum period in Hatay, Turkey. Nigerian Journal of Clinical Practice. 2018; 21(11):1525-30. [PMID]
- Hutton G. The effect of maternal-newborn ill-health on households: Economic vulnerability and social implications [Internet]. 2006 [Updated 2006]. Available from: https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/9241594489/en/
- Smith MP. Postnatal concerns of mothers: An update. Midwifery. 1989; 5(4):182-8. [DOI:10.1016/s0266-6138(89)80005-1] [PMID]
- Hung CH. Postpartum stress as a predictor of women’s minor psychiatric morbidity. Community Mental Health Journal. 2007; 43(1):1-12. [DOI:10.1007/s10597-006-9066-3] [PMID]
- George L. Lack of preparedness: Experiences of first-time mothers. MCN, The American Journal of Maternal/Child Nursing. 2005; 30(4):251-5. [DOI:10.1097/00005721-200507000-00009] [PMID]
- Hung CH. Correlates of first-time mothers’ postpartum stress. Kaohsiung Journal of Medical Sciences. 2006; 22(10):500-7. [DOI:10.1016/S1607-551X(09)70344-4]
- Hung CH. Revalidation of the postpartum stress scale. Journal of Clinical Nursing. 2006; 15(6):718-25. [DOI:10.1111/j.1365-2702.2006.01350.x] [PMID]
- Hung CH, Lin CJ, Stocker J, Yu CY. Predictors of postpartum stress. Journal of Clinical Nursing. 2011; 20(5-6):666-74. [DOI:10.1111/j.1365-2702.2010.03555.x] [PMID]
- Rahimi G, Sharghi A, Haj Mirzaiee M, Tazakkori Z. [Study of correlation between maternal depression and neonatal anthropometric measurements (Persian)]. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2013; 16(55):1-6. [DOI:10.22038/IJOGI.2013.1172]
- Pao Ch, Guintivano J, Santos H, Meltzer-Brody S. Postpartum depression and social support in a racially and ethnically diverse population of women. Archives of Women’s Mental Health. 2019; 22(1):105-14. [DOI:10.1007/s00737-018-0882-6] [PMID] [PMCID]
- Pham D, Cormick G, Amyx MM, Gibbons L, Doty M, Brown A, et al. Factors associated with postpartum depression in women from low socioeconomic level in Argentina: A hierarchical model approach. Journal of Affective Disorders. 2018; 227:731-8. [DOI:10.1016/j.jad.2017.11.091] [PMID] [PMCID]
- Sadock BJ, Sadock VA. Kaplan & Sadock’s Pocket Handbook of Clinical Psychiatry. Philadelphia: Lippincott Williams & Wilkins (LWW); 2018. https://www.amazon.com/Kaplan-Sadocks-Handbook-Clinical-Psychiatry/dp/1605472646
- Ahmadi Kani Golzar A, GoliZadeh Z. [Validation of Edinburgh Postpartum Depression Scale (EPDS) for screening postpartum depression in Iran (Persian)]. Iranian Journal of Psychiatric Nursing. 2015; 3(3):1-10. http://ijpn.ir/article-1-611-en.html
- Amir Ali Akbari S, Vameghi R, Sajedi F, Sajjadi H, Alavimajd H, Hajighasemali S. [Relationship between socio-economic status, perceived stress, social support and domestic violence with women’s depression in reproductive age using path analysis (Persian)]. Iranian Journal of Health Education and Health Promotion. 2016; 3(4):391-401. Persian. http://journal.ihepsa.ir/article-1-377-en.html
- Ghaedrahmati M, Kazemi A, Kheirabadi GR, Ebrahimi A, Bahrami M. Postpartum depression risk factors: A narrative review. Journal of Education and Health Promotion. 2017; 6:60. [PMID] [PMCID]
- Vaezi A, Soojoodi F, Tehrani Banihashemi A, Nojomi M. The association between social support and postpartum depression in women: A cross sectional study. Women and Birth. 2019; 32(2):e238-42. [DOI:10.1016/j.wombi.2018.07.014] [PMID]
- Moore N. The violent birth of the mother and the baby blues. Psychodynamic Practice. 2018; 24(1):60-3. [DOI:10.1080/14753634.2017.1400737]
- Manshoori A, Bidaki R, Esmaily H. Frequency of postpartum depression and its related factors in women referred to health centers in Rafsanjan, Iran, in 2015. Journal of Occupational Health and Epidemiology. 2017; 6(1):17-24. [DOI:10.18869/acadpub.johe.6.1.17]
- Saberi N, Amir Ali Akbari S, Mahmoodi Z, Nasiri M. [Model for the relationship between sexual function and social determinants of health: Path analysis (Persian)]. Koomesh. 2018; 20(2):391-402. http://koomeshjournal.semums.ac.ir/article-1-4096-en.html
- Noury R, Karimi N, Mohammadi M. [Relationship between prenatal depression with social support and marital satisfaction (Persian)]. Sarem Journal of Reproductive Medicine. 2017; 2(3):153-7. [DOI:10.29252/sjrm.1.4.153]
- Simonič B, Poljanec A. Building motherhood in the young mothers’ group. Child Care in Practice. 2014; 20(3):270-85. [DOI:10.1080/13575279.2013.875461]
- Negron R, Martin A, Almog M, Balbierz A, Howell EA. Social support during the postpartum period: Mothers’ views on needs, expectations, and mobilization of support. Maternal and Child Health Journal. 2013; 17(4):616-23. [DOI:10.1007/s10995-012-1037-4] [PMID] [PMCID]
- Bakhtiyari M, Emaminaeini M, Hatami H, Khodakarim S, Sahaf R. [Depression and perceived social support in the elderly (Persian)]. Salmand: Iranian Journal of Ageing. 2017; 12(2):192-207. [DOI:10.21859/sija-1202192]
- Gruen DS. Postpartum depression: A debilitating yet often unassessed problem. Health & Social Work. 1990; 15(4):261-70. [DOI:10.1093/hsw/15.4.261] [PMID]
- Hopkins J, Campbell SB. Development and validation of a scale to assess social support in the postpartum period. Archives of Women’s Mental Health. 2008; 11(1):57-65. [DOI:10.1007/s00737-008-0212-5] [PMID]
- Ghaljeh M, Rezaee N, Mardani M, Ghasemi R. [Postpartum depression and some related factors (Persian)]. Sadra Medical Journal. 2013; 1(1):23-8. https://smsj.sums.ac.ir/article_43976.html
- Ngo LTH, Chou HF, Gau ML, Liu CY. Breastfeeding self-efficacy and related factors in postpartum Vietnamese women. Midwifery. 2019; 70:84-91. [DOI:10.1016/j.midw.2018.12.014] [PMID]
- Gao Ll, Sun K, Chan SWC. Social support and parenting self-efficacy among Chinese women in the perinatal period. Midwifery. 2014; 30(5):532-8. [DOI:10.1016/j.midw.2013.06.007] [PMID]
- Li Y, Long Z, Cao D, Cao F. Social support and depression across the perinatal period: A longitudinal study. Journal of Clinical Nursing. 2017; 26(17-18):2776-83. [DOI:10.1111/jocn.13817] [PMID]
- Nazari S, Salari P, Mazlom SR, Mahram B. [Comparison of social support in the first and second month of postpartum in multiparous (Persian)]. Community Health Journal. 2014; 8(2):1-9. http://chj.rums.ac.ir/article_45717.html
- Shafiee M, Davoodyzade Jolgeh H, Dabirifard M, Dabirifard S, Shafiee M. [The relationship between social support and postpartum depression in mothers with premature newborn infants: A critical survey (Persian)]. Tolooebehdasht. 2018; 17(4):81-93. [DOI:10.18502/tbj.v17i4.188]
- Azimi M, Fahami F, Mohamadirizi S. [The relationship between perceived social support in the first pregnancy and fear of childbirth (Persian)]. Iranian Journal of Nursing and Midwifery Research. 2018; 23(3):235-9. [DOI:10.4103/ijnmr.IJNMR_170_16] [PMID] [PMCID]
- Cheng CY, Pickler RH. Effects of stress and social support on postpartum health of Chinese mothers in the United States. Research in Nursing & Health. 2009; 32(6):582-91. [DOI:10.1002/nur.20356] [PMID]
- Strelow B, Fellows N, Fink SR, O’Laughlin DJ, Radke G, Stevens J, et al. Postpartum depression in older women. Journal of the American Academy of Physician Assistants. 2018; 31(3):15-8. [DOI:10.1097/01.JAA.0000530288.83376.8e] [PMID]
- Guin G, Rawat S. Prevalence of postpartum depression and association with risk factors in a tertiary care hospital. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2018; 7(3):1094-100. [DOI:10.18203/2320-1770.ijrcog20180899]
Article Type : Applicable |
Subject:
Special
Received: 2021/03/7 | Accepted: 2021/03/20 | Published: 2021/03/20
Received: 2021/03/7 | Accepted: 2021/03/20 | Published: 2021/03/20
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |


.jpg)
