Fri, Apr 26, 2024
Volume 31, Issue 2 (3-2021)
JHNM 2021, 31(2): 76-84 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yosefi Z, Afshar M, Mirbagher Ajorpaz N, Sadat Z. The Effect of Training Based on James Brown Model on Self-efficacy in Adolescents with Type 1 Diabetes Mellitus. JHNM 2021; 31 (2) :76-84
URL: http://hnmj.gums.ac.ir/article-1-1590-en.html
URL: http://hnmj.gums.ac.ir/article-1-1590-en.html
1- Nursing (MSN), Department Of Nursing And Midwifery, Trauma Nursing Research Center, Kashan University of Medical Sciences, Kashan, Iran
2- Associate Professor, Department Of Nursing And Midwifery, Trauma Nursing Research Center, Department of Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran
3- Assistant Professor, Department Of Nursing And Midwifery, Autoimmune Diseases Research Center, Department of Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran , mirbagher_n@kaums.ac.ir
2- Associate Professor, Department Of Nursing And Midwifery, Trauma Nursing Research Center, Department of Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran
3- Assistant Professor, Department Of Nursing And Midwifery, Autoimmune Diseases Research Center, Department of Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran , mirbagher_n@kaums.ac.ir
Full-Text [PDF 656 kb]
(819 Downloads)
| Abstract (HTML) (1573 Views)
Full-Text: (974 Views)
Introduction
ype 1 Diabetes Mellitus (T1DM) is one of the most frequent chronic diseases among children and adolescents. In recent decades, there has been a significant increase in the prevalence of diabetes worldwide, as 415 million people in the world are affected by this disease [1]. For example, in Iran, over 4.5 million people are affected by diabetes mellitus, and over 50000 patients are children and adolescents [2, 3]. Diabetes mellitus is a self-management disease, meaning that the patients are responsible for most of their care plan. Scholars believed that the main approach to blood glucose management and the prevention of disease complications is patients’ active roles in their health care through self-care behaviors [4, 5].
Self-efficacy is the main factor related to self-care behaviors [5, 6]. Self-efficacy is a fundamental concept in Albert Bandura’s social cognitive theory developed in 1997 [6]. Based on this theory, self-efficacy is an individual’s belief in his/her ability to achieve goals through individual efforts [7]. Self-efficacy is a crucial factor regarding behavior change among diabetic patients [2, 8] and plays a vital role in the treatment of chronic diseases in general [9]. However, evidence indicates that self-efficacy scores are low to moderate among adolescents with T1DM [10].
In the modern management of diabetes, the patient oversees the disease and complication management, and healthcare professionals provide patient education to improve self-efficacy behaviors [11]. Educational strategies underscore patients’ roles in the management of diseases and enhance self-efficacy behaviors. These efforts lead to healthcare cost-effectiveness, reduce hospitalizations, and prevent chronic disease complications [12]. Educational strategies based on the model created by James Brown et al. have attracted the researchers’ interest and are considered adequate to improve patients’ self-efficacy [12, 13]. Based on this model, learners are located at the core of the learning process, indicating that their characteristics, including their interests and capacities, are the critical components of education [13]. The emphasis in this model is on the identification and modification of learning groups, educational goals, education timings, teaching methods, educational environments, and the use of educational tools [14]. Some advantages of this model are the use of diverse methods of education, such as games, simulations, videos, and group discussions—compatible with the learners’ interests. There is also a specific focus on the educational environment; for example, education is offered in recreational environments, such as parks [13, 14].
One study indicates that this model has positive effects on the knowledge and attitudes of patients with type 2 diabetes mellitus [15]. Another study showed that this model had improved women’s experience about reproductive and sexual health [16]. In Iran, no published research was found about training this model to enhance self-efficacy in adolescents with diabetes. Because self-efficacy in adolescents with type 1 diabetes has received less attention and this disease has adverse effects on the individual, family, and society, the current study was conducted to investigate the impact of education based on James Brown’s model on self-efficacy in adolescents with T1DM.
Materials and Methods
This study is a randomized controlled clinical trial. This study was conducted in Diabetes Center, Kashan, Iran, from January 2018 to September 2018. Based on results of the study by Moein et al. (S1 and S2 were respectively equal to 14.49 and 17.1) [7], α and β were respectively equal to 0.05 and 0.2 with a type 1 error of 0.05 and a power of 0.85, and finally based on the Pocock’s sample size formula [17], the number of participants in each group was estimated to be 32. Considering the 25% attrition, the final sample size for each group was calculated to be 40.
The inclusion criteria were the participants aged 13–19 years, had a definitive diagnosis of type 1 diabetes mellitus by an endocrinologist for at least six months, were not currently or previously participating in educational self-care programs based on the self-report of the patient and her/his family, did not have any other chronic or disabling diseases, and could independently complete the survey. The exclusion criteria for the participants were missing three or more educational sessions and diagnosis of other chronic or disabling conditions throughout the study. The participants were randomly assigned to the intervention (n=40) and control (n=40) groups by randomization block included 4 blocks of 10 (simple allocation using www.sealedenvelope.com) [18]. All participants voluntarily accepted to participate in the study.
The participants in both groups received routine care for T1DM. In addition to the routine care, the intervention group was provided with educational sessions. These sessions were held for 60 minutes twice a week for 4 weeks. Educational sessions were based on self-care behaviors grounded in James Brown et al. educational model [13]. A total of 8 sessions were held early in the morning on Mondays and Wednesdays in a Diabetes Center, Kashan City, Iran. It is noteworthy that the sessions were held in the summer season, and the adolescents did not have any educational activities at school at this time. The sessions were face-to-face and included group discussions and questions/answers between the first researcher and the participants. Educational materials that were used in the sessions included PowerPoints, videos, and pamphlets. Based on the model, 4 steps of addressing educational goals, educational conditions, educational resources, and academic outcomes were followed (Table 1).
.jpg)
The study measures included a sociodemographic questionnaire (age, sex, daily insulin intake, education, disease duration, treatment method, birth order) and the Diabetes Management Self-Efficacy (DMSE) instrument. The DMSE was developed, and its content validity was assessed by Bijl et al. (1999). The instrument is a 10-point Likert-type scale and consists of 20 items and 4 subscales. The subscales include nutrition (9 items), blood glucose monitoring (4 items), physical activity (4 items), and medical treatment (3 items). The total score ranges from 0 to 200. A higher score indicates a greater level of self-efficacy. Reliability for the instrument was reported 0.79 [19]. The Persian version of DMSE has been shown to have adequate reliability and validity by Haghayegh et al. [20]. In the current study, the tool’s validity was confirmed through content validity and the approval of 10 experts in this field. In a pilot study of 20 diabetic adolescents (except the participants in this study), the Cronbach alpha was calculated in subscales between 0.86 to 0.90.
The first researcher contacted the participants in the intervention group twice a week to remind them to practice the trained activities and to answer their questions. The researcher’s contact number was also provided to the participants. The researcher informed the participants to contact her if any related questions or concerns came up during the course of the study. Throughout the study, the control group only received routine care for diabetic patients.
Handouts consisting of the educational materials for the intervention group were provided for the control group’s participants after the end of the study.
To answer the questions, in addition to the adolescents, the parents also completed the informed consent form. The survey was completed by the participants before, immediately after the last session, and one month after the intervention. A month after the intervention, the intervention and control groups’ participants were asked to report to the Diabetes Center and complete the survey. The researcher contacted those participants who did not report to the center and scheduled to meet the participants at a convenient time and place to complete the survey.
In addition to adolescents, written informed consent was obtained from their parents. The normal distribution of the data and variables was verified by the Kolmogorov-Smirnov test. Continuous demographic variables were reported with mean and standard deviation and categorical demographic variables with frequencies and percentages. At the beginning of the study, the intervention and control groups were compared in terms of their sociodemographic characteristics using the Chi-square and Independent samples t-test. The repeated measures ANOVA was used to compare the mean scores of self-efficacy and its subscales at three time-points (before, immediately after the last session, and one month after the intervention). Analysis of Covariance (ANCOVA) was used to compare the mean scores of self-efficacy between the two groups. The statistical analysis was performed using SPSS for Windows, version 16.0 (SPSS Inc., Chicago, IL, USA), and the level of significance was set at 0.05.
Results
In the intervention group, 5 patients were excluded because of their absence in 3 or more educational sessions. In the control group, 5 patients were excluded due to a failure to complete the questionnaire at the end of the study. Thus, the study was completed by 35 participants in each group (Figure 1). The sociodemographic characteristics of the two groups are presented in Table 2.
.jpg)
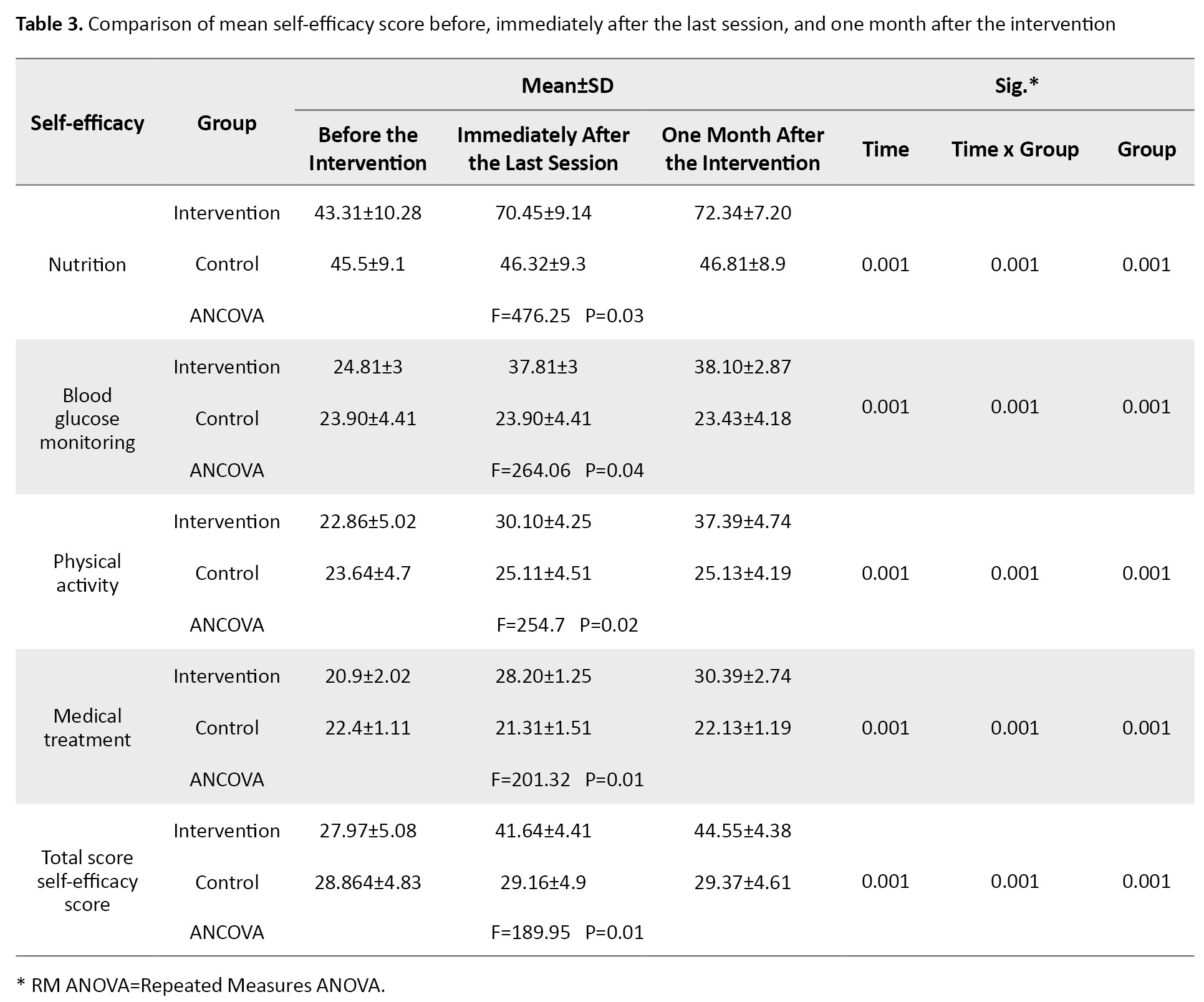
There was no significant difference between the two groups in terms of their sociodemographic characteristics. Table 2 is related to the results of repeated measures ANOVA in the intervention group and showed that the mean scores of self-efficacy and its subscales (nutrition, blood glucose monitoring, physical activity, and medical treatment) increased over the three time-points (P<0.05). Immediately after the last session and one month after the intervention, the mean±SD scores of self-efficacy were 27.97±5.08, 41.46±4.41, and 44.55 ±4.38, respectively, and in the control group were 28.864±4.83, 29.1±4.9, and 29.37±4.61, respectively. The results of the ANCOVA test also showed that there was a significant difference (P<0.05) between the two groups’ mean scores of self-efficacy (Table 3).
Discussion
The findings showed significant differences between the intervention and control groups in terms of their self-efficacy scores and its subscales over time (immediately after the last session and one month after the intervention). These findings indicated that the educational intervention based on James Brown’s model effectively improved self-efficacy among the participants’ disease management. Our results were in line with Reisi et al. [21]. They found that educational programs effectively improved self-efficacy and self-care behaviors among patients with type 2 diabetes mellitus. However, their educational intervention was not based on the model used in the present study.
Evidence indicated several interventions that may be positive in the improvement of self-efficacy among patients. Khavasi et al. reported that peer education positively affects type 2 diabetic patients’ self-efficacy [22]. A study also found that education based on Bandura’s social learning theory positively affected general self-efficacy and type 2 diabetic patients’ self-efficacy [6].
Consistent with our findings, Ghazanfari et al. reported that an educational program based on James Brown’s model positively affects knowledge and attitudes among patients with type 2 diabetes [15]. Also, research states that education based on this model improves the knowledge regarding reproductive and sexual health among women participating in marriage counseling programs [16]. Ayele et al. supported the significance of education in enhancing self-efficacy and self-care behaviors among diabetic patients [23]. A study also reported that education and counseling could improve self-care behaviors among patients with type 2 diabetes mellitus [24]. This consistency is that in all studies, items such as diet and physical activity, how to control blood sugar, and medical care have been taught in different ways, which is one of the subscales of self-efficacy. The studies are consistent in terms of the number of sessions and the educational content.
In line with James Brown’s model, researchers believed that educational programs could be effective in patients with diabetes mellitus if they are planned based on specific goals and if learning objectives are defined with patients’ and their caregivers’ engagement [25, 26, 27, 28].
The findings indicated that in the intervention group, the self-efficacy subscales (nutrition, blood glucose monitoring, physical activity, and medical treatment) were also improved over time (immediately after the last session and one month after the intervention).
Kazeminezhad et al. found that after education regarding self-care behaviors, the hemoglobin A1C and Fasting Blood Sugar (FBS) were significantly decreased [29]. Farmahini Farahani et al. reported that multimedia education effectively improves knowledge and self-care behaviors among women with type 2 diabetes mellitus [30]. Azizi et al. also indicated that education based on a self-care model effectively manages diabetic complications, medication use, and hemoglobin A1C in adolescents with T1DM [31]. Shabibi et al. stated that the education based on the health belief model was significant regarding improving self-care behaviors and nutrition, physical activity and exercise, and the management of early and late complications of diabetes [32]. These studies, like the present study, have used items that are important in the James Brown model, such as experiential learning, verbal encouragement, goal setting, and role-playing, the results of which are consistent with the present study. Sacco et al. indicated that phone contacts for a follow-up enhanced adherence to the exercise program, foot care, and nutrition modification among diabetic patients [33].
Several studies addressed effective educational and psychological interventions in diabetic patients. Their findings showed that the most effective educational methods related to self-efficacy in diabetic patients involve preset goals and is grounded in principles of empowerment and problem solving [34, 35]. Other studies indicated that education should be tailored to the patient’s specific needs and conditions, including age, type and severity of diabetes, lifestyle, and culture [36, 37, 38]. These statements are congruent with James Brown’s model. The International Society for Pediatric and Adolescent Diabetes (ISPAD) also supports these statements indicating that education of diabetic patients, especially children and adolescents, needs to be organized based on patients’ attitudes, belief systems, preferred learning methods, capacities, learning preparedness, and goals [39].
The strengths of the study included the use of an educational model to increase adolescent self-efficacy and also to use games, simulations, and role models for the patient and her/his family education. This research was limited to the diabetic adolescents referred to a diabetes center in Kashan. Questionnaire completion based on self-reporting was another limitation of this study.
We found that education based on James Brown’s model can improve self-efficacy among adolescents with T1DM. Considering the high prevalence of diabetes and its complications, healthcare researchers and professionals need to find strategies to integrate cost-effective and convenient interventions for improving evidence-based practice regarding the management of diabetes. We suggest education based on the James Brown model for improving self-efficacy among adolescents with T1DM.
al Considerations
Compliance with ethical guidelines
The Ethics Review Committee of Kashan University of Medical Sciences approved the study (IR.KAUMS.NUHEPM.REC.2018.032). The participants provided written informed consent and were informed of their right to withdraw from the study at any time. This trail was also registered at www.irct.ir (Trial Registration Number: IRCT20111210008348N39.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Concept and design: Zahra Yosefi, Neda Mirbagher Ajorpaz; Data collection: Zahra Yosefi; Analysis and interpretation of data: Neda Mirbagher Ajorpaz; Manuscript draft: Mohammad Afshar; Critical revision of the manuscript: Zahra Yosefi, Neda Mirbagher Ajorpaz, Mohammad Afshar; Final approval of the manuscript: all aythors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We would like to thank all patients participated in the study. This study was supported by the Kashan University of Medical Sciences.
References
ype 1 Diabetes Mellitus (T1DM) is one of the most frequent chronic diseases among children and adolescents. In recent decades, there has been a significant increase in the prevalence of diabetes worldwide, as 415 million people in the world are affected by this disease [1]. For example, in Iran, over 4.5 million people are affected by diabetes mellitus, and over 50000 patients are children and adolescents [2, 3]. Diabetes mellitus is a self-management disease, meaning that the patients are responsible for most of their care plan. Scholars believed that the main approach to blood glucose management and the prevention of disease complications is patients’ active roles in their health care through self-care behaviors [4, 5].
Self-efficacy is the main factor related to self-care behaviors [5, 6]. Self-efficacy is a fundamental concept in Albert Bandura’s social cognitive theory developed in 1997 [6]. Based on this theory, self-efficacy is an individual’s belief in his/her ability to achieve goals through individual efforts [7]. Self-efficacy is a crucial factor regarding behavior change among diabetic patients [2, 8] and plays a vital role in the treatment of chronic diseases in general [9]. However, evidence indicates that self-efficacy scores are low to moderate among adolescents with T1DM [10].
In the modern management of diabetes, the patient oversees the disease and complication management, and healthcare professionals provide patient education to improve self-efficacy behaviors [11]. Educational strategies underscore patients’ roles in the management of diseases and enhance self-efficacy behaviors. These efforts lead to healthcare cost-effectiveness, reduce hospitalizations, and prevent chronic disease complications [12]. Educational strategies based on the model created by James Brown et al. have attracted the researchers’ interest and are considered adequate to improve patients’ self-efficacy [12, 13]. Based on this model, learners are located at the core of the learning process, indicating that their characteristics, including their interests and capacities, are the critical components of education [13]. The emphasis in this model is on the identification and modification of learning groups, educational goals, education timings, teaching methods, educational environments, and the use of educational tools [14]. Some advantages of this model are the use of diverse methods of education, such as games, simulations, videos, and group discussions—compatible with the learners’ interests. There is also a specific focus on the educational environment; for example, education is offered in recreational environments, such as parks [13, 14].
One study indicates that this model has positive effects on the knowledge and attitudes of patients with type 2 diabetes mellitus [15]. Another study showed that this model had improved women’s experience about reproductive and sexual health [16]. In Iran, no published research was found about training this model to enhance self-efficacy in adolescents with diabetes. Because self-efficacy in adolescents with type 1 diabetes has received less attention and this disease has adverse effects on the individual, family, and society, the current study was conducted to investigate the impact of education based on James Brown’s model on self-efficacy in adolescents with T1DM.
Materials and Methods
This study is a randomized controlled clinical trial. This study was conducted in Diabetes Center, Kashan, Iran, from January 2018 to September 2018. Based on results of the study by Moein et al. (S1 and S2 were respectively equal to 14.49 and 17.1) [7], α and β were respectively equal to 0.05 and 0.2 with a type 1 error of 0.05 and a power of 0.85, and finally based on the Pocock’s sample size formula [17], the number of participants in each group was estimated to be 32. Considering the 25% attrition, the final sample size for each group was calculated to be 40.
The inclusion criteria were the participants aged 13–19 years, had a definitive diagnosis of type 1 diabetes mellitus by an endocrinologist for at least six months, were not currently or previously participating in educational self-care programs based on the self-report of the patient and her/his family, did not have any other chronic or disabling diseases, and could independently complete the survey. The exclusion criteria for the participants were missing three or more educational sessions and diagnosis of other chronic or disabling conditions throughout the study. The participants were randomly assigned to the intervention (n=40) and control (n=40) groups by randomization block included 4 blocks of 10 (simple allocation using www.sealedenvelope.com) [18]. All participants voluntarily accepted to participate in the study.
The participants in both groups received routine care for T1DM. In addition to the routine care, the intervention group was provided with educational sessions. These sessions were held for 60 minutes twice a week for 4 weeks. Educational sessions were based on self-care behaviors grounded in James Brown et al. educational model [13]. A total of 8 sessions were held early in the morning on Mondays and Wednesdays in a Diabetes Center, Kashan City, Iran. It is noteworthy that the sessions were held in the summer season, and the adolescents did not have any educational activities at school at this time. The sessions were face-to-face and included group discussions and questions/answers between the first researcher and the participants. Educational materials that were used in the sessions included PowerPoints, videos, and pamphlets. Based on the model, 4 steps of addressing educational goals, educational conditions, educational resources, and academic outcomes were followed (Table 1).
.jpg)
The study measures included a sociodemographic questionnaire (age, sex, daily insulin intake, education, disease duration, treatment method, birth order) and the Diabetes Management Self-Efficacy (DMSE) instrument. The DMSE was developed, and its content validity was assessed by Bijl et al. (1999). The instrument is a 10-point Likert-type scale and consists of 20 items and 4 subscales. The subscales include nutrition (9 items), blood glucose monitoring (4 items), physical activity (4 items), and medical treatment (3 items). The total score ranges from 0 to 200. A higher score indicates a greater level of self-efficacy. Reliability for the instrument was reported 0.79 [19]. The Persian version of DMSE has been shown to have adequate reliability and validity by Haghayegh et al. [20]. In the current study, the tool’s validity was confirmed through content validity and the approval of 10 experts in this field. In a pilot study of 20 diabetic adolescents (except the participants in this study), the Cronbach alpha was calculated in subscales between 0.86 to 0.90.
The first researcher contacted the participants in the intervention group twice a week to remind them to practice the trained activities and to answer their questions. The researcher’s contact number was also provided to the participants. The researcher informed the participants to contact her if any related questions or concerns came up during the course of the study. Throughout the study, the control group only received routine care for diabetic patients.
Handouts consisting of the educational materials for the intervention group were provided for the control group’s participants after the end of the study.
To answer the questions, in addition to the adolescents, the parents also completed the informed consent form. The survey was completed by the participants before, immediately after the last session, and one month after the intervention. A month after the intervention, the intervention and control groups’ participants were asked to report to the Diabetes Center and complete the survey. The researcher contacted those participants who did not report to the center and scheduled to meet the participants at a convenient time and place to complete the survey.
In addition to adolescents, written informed consent was obtained from their parents. The normal distribution of the data and variables was verified by the Kolmogorov-Smirnov test. Continuous demographic variables were reported with mean and standard deviation and categorical demographic variables with frequencies and percentages. At the beginning of the study, the intervention and control groups were compared in terms of their sociodemographic characteristics using the Chi-square and Independent samples t-test. The repeated measures ANOVA was used to compare the mean scores of self-efficacy and its subscales at three time-points (before, immediately after the last session, and one month after the intervention). Analysis of Covariance (ANCOVA) was used to compare the mean scores of self-efficacy between the two groups. The statistical analysis was performed using SPSS for Windows, version 16.0 (SPSS Inc., Chicago, IL, USA), and the level of significance was set at 0.05.
Results
In the intervention group, 5 patients were excluded because of their absence in 3 or more educational sessions. In the control group, 5 patients were excluded due to a failure to complete the questionnaire at the end of the study. Thus, the study was completed by 35 participants in each group (Figure 1). The sociodemographic characteristics of the two groups are presented in Table 2.
.jpg)
There was no significant difference between the two groups in terms of their sociodemographic characteristics. Table 2 is related to the results of repeated measures ANOVA in the intervention group and showed that the mean scores of self-efficacy and its subscales (nutrition, blood glucose monitoring, physical activity, and medical treatment) increased over the three time-points (P<0.05). Immediately after the last session and one month after the intervention, the mean±SD scores of self-efficacy were 27.97±5.08, 41.46±4.41, and 44.55 ±4.38, respectively, and in the control group were 28.864±4.83, 29.1±4.9, and 29.37±4.61, respectively. The results of the ANCOVA test also showed that there was a significant difference (P<0.05) between the two groups’ mean scores of self-efficacy (Table 3).
Discussion
The findings showed significant differences between the intervention and control groups in terms of their self-efficacy scores and its subscales over time (immediately after the last session and one month after the intervention). These findings indicated that the educational intervention based on James Brown’s model effectively improved self-efficacy among the participants’ disease management. Our results were in line with Reisi et al. [21]. They found that educational programs effectively improved self-efficacy and self-care behaviors among patients with type 2 diabetes mellitus. However, their educational intervention was not based on the model used in the present study.
Evidence indicated several interventions that may be positive in the improvement of self-efficacy among patients. Khavasi et al. reported that peer education positively affects type 2 diabetic patients’ self-efficacy [22]. A study also found that education based on Bandura’s social learning theory positively affected general self-efficacy and type 2 diabetic patients’ self-efficacy [6].
Consistent with our findings, Ghazanfari et al. reported that an educational program based on James Brown’s model positively affects knowledge and attitudes among patients with type 2 diabetes [15]. Also, research states that education based on this model improves the knowledge regarding reproductive and sexual health among women participating in marriage counseling programs [16]. Ayele et al. supported the significance of education in enhancing self-efficacy and self-care behaviors among diabetic patients [23]. A study also reported that education and counseling could improve self-care behaviors among patients with type 2 diabetes mellitus [24]. This consistency is that in all studies, items such as diet and physical activity, how to control blood sugar, and medical care have been taught in different ways, which is one of the subscales of self-efficacy. The studies are consistent in terms of the number of sessions and the educational content.
In line with James Brown’s model, researchers believed that educational programs could be effective in patients with diabetes mellitus if they are planned based on specific goals and if learning objectives are defined with patients’ and their caregivers’ engagement [25, 26, 27, 28].
The findings indicated that in the intervention group, the self-efficacy subscales (nutrition, blood glucose monitoring, physical activity, and medical treatment) were also improved over time (immediately after the last session and one month after the intervention).
Kazeminezhad et al. found that after education regarding self-care behaviors, the hemoglobin A1C and Fasting Blood Sugar (FBS) were significantly decreased [29]. Farmahini Farahani et al. reported that multimedia education effectively improves knowledge and self-care behaviors among women with type 2 diabetes mellitus [30]. Azizi et al. also indicated that education based on a self-care model effectively manages diabetic complications, medication use, and hemoglobin A1C in adolescents with T1DM [31]. Shabibi et al. stated that the education based on the health belief model was significant regarding improving self-care behaviors and nutrition, physical activity and exercise, and the management of early and late complications of diabetes [32]. These studies, like the present study, have used items that are important in the James Brown model, such as experiential learning, verbal encouragement, goal setting, and role-playing, the results of which are consistent with the present study. Sacco et al. indicated that phone contacts for a follow-up enhanced adherence to the exercise program, foot care, and nutrition modification among diabetic patients [33].
Several studies addressed effective educational and psychological interventions in diabetic patients. Their findings showed that the most effective educational methods related to self-efficacy in diabetic patients involve preset goals and is grounded in principles of empowerment and problem solving [34, 35]. Other studies indicated that education should be tailored to the patient’s specific needs and conditions, including age, type and severity of diabetes, lifestyle, and culture [36, 37, 38]. These statements are congruent with James Brown’s model. The International Society for Pediatric and Adolescent Diabetes (ISPAD) also supports these statements indicating that education of diabetic patients, especially children and adolescents, needs to be organized based on patients’ attitudes, belief systems, preferred learning methods, capacities, learning preparedness, and goals [39].
The strengths of the study included the use of an educational model to increase adolescent self-efficacy and also to use games, simulations, and role models for the patient and her/his family education. This research was limited to the diabetic adolescents referred to a diabetes center in Kashan. Questionnaire completion based on self-reporting was another limitation of this study.
We found that education based on James Brown’s model can improve self-efficacy among adolescents with T1DM. Considering the high prevalence of diabetes and its complications, healthcare researchers and professionals need to find strategies to integrate cost-effective and convenient interventions for improving evidence-based practice regarding the management of diabetes. We suggest education based on the James Brown model for improving self-efficacy among adolescents with T1DM.
al Considerations
Compliance with ethical guidelines
The Ethics Review Committee of Kashan University of Medical Sciences approved the study (IR.KAUMS.NUHEPM.REC.2018.032). The participants provided written informed consent and were informed of their right to withdraw from the study at any time. This trail was also registered at www.irct.ir (Trial Registration Number: IRCT20111210008348N39.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Concept and design: Zahra Yosefi, Neda Mirbagher Ajorpaz; Data collection: Zahra Yosefi; Analysis and interpretation of data: Neda Mirbagher Ajorpaz; Manuscript draft: Mohammad Afshar; Critical revision of the manuscript: Zahra Yosefi, Neda Mirbagher Ajorpaz, Mohammad Afshar; Final approval of the manuscript: all aythors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We would like to thank all patients participated in the study. This study was supported by the Kashan University of Medical Sciences.
References
- Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: A review of current evidence. Diabetologia. 2019; 62(1):3-16. [DOI:10.1007/s00125-018-4711-2] [PMID]
- Esteghamati AR, Larijani B, Haji Aghajani M, Ghaemi F, Kermanchi J, Shahrami A, et al. Diabetes in Iran: Prospective analysis from first nationwide diabetes report of National Program for Prevention and Control of Diabetes (NPPCD-2016). Scientific Reports. 2017; 7(1):13461. [DOI:10.1038/s41598-017-13379-z] [PMID] [PMCID]
- Murillo M, Bel J, Pérez J, Corripio R, Carreras G, Herrero X, et al. Health-Related Quality of Life (HRQOL) and its associated factors in children with Type 1 Diabetes Mellitus (T1DM). BMC Pediatrics. 2017; 17(1):16. [DOI:10.1186/s12887-017-0788-x] [PMID] [PMCID]
- Abubakari AR, Cousins R, Thomas C, Sharma D, Naderali EK. Sociodemographic and clinical predictors of self-management among people with poorly controlled type 1 and type 2 diabetes: The role of illness perceptions and self-efficacy. Journal of Diabetes Research. 2016; 2016:6708164. [DOI:10.1155/2016/6708164] [PMID] [PMCID]
- Mayberry LS, Osborn CY. Family involvement is helpful and harmful to patients’ self-care and glycemic control. Patient Education and Counseling. 2014; 97(3):418-25. [DOI:10.1016/j.pec.2014.09.011] [PMID] [PMCID]
- Eshghi Motlagh A, Babazadeh R, Akhlaghi F, Esmaily H. Effect of an educational intervention program based on Bandura’s self-efficacy theory on self-care, self-efficacy, and blood sugar levels in mothers with pre-diabetes during pregnancy. Evidence Based Care Journal. 2019; 9(2):53-64. [DOI:10.22038/EBCJ.2019.37173.1959]
- Moein M, Aghajani M, Mirbagher Ajorpaz N, Khorasanifar L. Effect of an empowerment program on self-efficacy of patients with type 2 diabetes. Iranian Red Crescent Medical Journal. 2016; 19(1):e29252. [DOI:10.5812/ircmj.29252]
- Rasbach LE, Volkening LK, Markowitz JT, Butler DA, Katz ML, Laffel LMB. Youth and parent measures of self-efficacy for continuous glucose monitoring: Survey psychometric properties. Diabetes Technology & Therapeutics. 2015; 17(5):327-34. [DOI:10.1089/dia.2014.0366] [PMID] [PMCID]
- Seyyedrasooli A, Parvan K, Valizadeh L, Rahmani A, Zare M, Izadi T. Self-efficacy in foot-care and effect of training: A single-blinded randomized controlled clinical trial. International Journal of Community Based Nursing and Midwifery. 2015; 3(2):141-9. [PMID] [PMCID]
- Chih AH, Jan CF, Shu SG, Lue BH. Self-efficacy affects blood sugar control among adolescents with type I diabetes mellitus. Journal of the Formosan Medical Association. 2010; 109(7):503-10. [DOI:10.1016/S0929-6646(10)60084-8]
- Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. Journal of Diabetes & Metabolic Disorders. 2013; 12(1):14. [DOI:10.1186/2251-6581-12-14] [PMID] [PMCID]
- Brown J, Bearman M, Kirby C, Molloy E, Colville D, Nestel D. Theory, a lost character? As presented in general practice education research papers. Medical Education. 2019; 53(5):443-57. [DOI:10.1111/medu.13793] [PMID]
- Brown J, Nestel D. Theories and myths in medical education: What is valued and who is served? Medical Education. 2020; 54(1):4-6. [DOI:10.1111/medu.14003] [PMID]
- Ebadi Fardaza F, Heidari H, Solhi M. Effect of educational intervention based on locus of control structure of attribution theory on self-care behavior of patients with type II diabetes. Medical Journal of the Islamic Republic of Iran. 2017; 31:116. [DOI:10.14196/mjiri.31.116] [PMID] [PMCID]
- Ghazanfari Z, Ghofranipour F, Rajab A, Ahmadi F. [The effect of educational program based on James Brown model on knowledge and attitude of type II diabetic patients (Persian)]. Daneshvar Medicine: Basic and Clinical Research Journal. 2006; 14(65):45-54. https://www.sid.ir/fa/journal/ViewPaper.aspx?ID=57841
- Khodakarami B, Aligholi S. [The effect of education based on James Brown pattern on knowledge of reproductive & sexual health in women participant marriage council classes in Hamadan (Persian)]. Avicenna Journal of Nursing and Midwifery Care. 2011; 19(1):52-62. http://nmj.umsha.ac.ir/article-1-1091-en.html
- Pocock SJ. Clinical trials: A practical approach. Chichester: John Wiley & Sons; 1983. https://books.google.com/books?id=Oj5rAAAAMAAJ&dq
- Sealed Envelope Ltd. Create a blocked randomisation list [Internet]. 2020 [Updated 2020]. Available from: https://www.sealedenvelope.com/simple-randomiser/v1/lists
- van der Bijl J, van Poelgeest-Eeltink A, Shortridge-Baggett L. The psychometric properties of the diabetes management self-efficacy scale for patients with type 2 diabetes mellitus. Journal of Advanced Nursing. 1999; 30(2):352-9. [DOI:10.1046/j.1365-2648.1999.01077.x] [PMID]
- Haghayegh SA, Ghasemi N, Neshardoost HT, Kajbaf MB, Khanbani M. [Psychometric properties of diabetes management (Persian)]. Iranian Journal of Endocrinology and Metabolism. 2010; 12(2):111-5. http://ijem.sbmu.ac.ir/article-1-789-en.html
- Reisi M, Javadzede H, Sharifirad GR, Mostafavi F, Tavassoli E, Imanzad M. Effects of an educational intervention on self-care and metabolic control in patients with type II diabetes. Journal of Client-Centered Nursing Care. 2017; 3(3):205-14. [DOI:10.32598/jccnc.3.3.205]
- Khavasi M, Masroor D, Varaei Sh, Joudaki K, Rezaei M, Rastegari Mehr B, et al. [The effect of peer education on diabetes self-efficacy in patients with type 2 diabetes: A randomized clinical trial (Persian)]. Journal of Knowledge & Health. 2016; 11(2):67-74. [DOI:10.22100/jkh.v11i2.1359]
- Ayele K, Tesfa B, Abebe L, Tilahun T, Girma E. Self care behavior among patients with diabetes in Harari, Eastern Ethiopia: The health belief model perspective. PloS One. 2012; 7(4):e35515. [[DOI:10.1371/journal.pone.0035515] [PMID] [PMCID]
- Gallegos EC, Ovalle-Berumen F, Gomez-Meza MV. Metabolic control of adults with type 2 diabetes mellitus through education and counseling. Journal of Nursing Scholarship. 2006; 38(4):344-51. [DOI:10.1111/j.1547-5069.2006.00125.x] [PMID]
- American Diabetes Association. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2018. Diabetes Care. 2018; 41(suppl 1):S13-27. [DOI:10.2337/dc18-S002] [PMID]
- Duca LM, Reboussin BA, Pihoker C, Imperatore G, Saydah Sh, Mayer-Davis E, et al. Diabetic ketoacidosis at diagnosis of Type 1 diabetes and glycemic control over time: The SEARCH for diabetes in youth study. Pediatric Diabetes. 2019; 20(2):172-9. [DOI:10.1111/pedi.12809] [PMID] [PMCID]
- Waller D, Johnston C, Molyneaux L, Brown-Singh L, Hatherly K, Smith L, et al. Glycemic control and blood glucose monitoring over time in a sample of young Australians with Type 1 diabetes: The role of personality. Diabetes Care. 2013; 36(10):2968-73. [DOI:10.2337/dc12-1743] [PMID] [PMCID]
- Mahdizadeh M, Peymam N, Taghipour A, Esmaily H, Mahdizadeh SM. Effect of health education program on promoting physical activity among diabetic women in Mashhad, Iran: Applying social cognitive theory. Journal of Research in Health Sciences. 2013; 13(1):90-7. [PMID]
- Kazeminezhad B, Taghinejad H, Borji M, Tarjoman A. The effect of self-care on glycated hemoglobin and fasting blood sugar levels on adolescents with diabetes. Journal of Comprehensive Pediatrics. 2018; 9(2):e62661. [DOI:10.5812/compreped.62661]
- Farmahini Farahani M, Purfarzad Z, Ghorbani M, Ghamari Zare Z, Ghorbani F. The impact of multimedia software support on the knowledge and self-care behaviors of patients with type 2 diabetes: A randomized clinical trial. Journal of Caring Sciences. 2016; 5(2):111-20. [DOI:10.15171/jcs.2016.012] [PMID] [PMCID]
- Azizi M, Arsalani N, Mohammadi Shahboulaghi F, Hosseinzadeh S, Rajab A. [The effect of self-care education on the control of diabetes complications, medications and HbA1C in adolescents with Type 1 diabetes (Persian)]. Journal of Hayat. 2017; 22(4):350-61. http://hayat.tums.ac.ir/article-1-1638-en.html
- Shabibi P, Abedzadeh Zavareh MS, Sayehmiri K, Qorbani M, Safari O, Rastegarimehr B, et al. Effect of educational intervention based on the Health Belief Model on promoting self-care behaviors of type-2 diabetes patients. Electronic Physician. 2017; 9(12):5960-8. [DOI:10.19082/5960] [PMID] [PMCID]
- Sacco WP, Bykowski CA, Mayhew LL, White KE. Educational attainment moderates the effect of a brief diabetes self-care intervention. Diabetes Research and Clinical Practice. 2012; 95(1):62-7. [DOI:10.1016/j.diabres.2011.08.027] [PMID]
- Ghoreishi MS, Vahedian-Shahroodi M, Jafari AR, Tehranid H. Self-care behaviors in patients with type 2 diabetes: Education intervention base on social cognitive theory. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2019; 13(3):2049-56. [DOI:10.1016/j.dsx.2019.04.045] [PMID]
- Qasim R, Masih S, Hussain M, Ali A, Khan A, Shah Y, et al. Effect of diabetic counseling based on conversation map as compared to routine counseling on diabetes management self-efficacy and diabetic distress among patients with diabetes in Pakistan: A randomized controlled trial (study protocol). BMC Public Health. 2019; 19(1):907. [DOI:10.1186/s12889-019-7266-3] [PMID] [PMCID]
- Choudhary P, Campbell F, Joule N, Kar P, Diabetes UK. A Type 1 diabetes technology pathway: Consensus statement for the use of technology in Type 1 diabetes. Diabetic Medicine. 2019; 36(5):531-8. [DOI:10.1111/dme.13933] [PMID]
- Ewers B, Vilsbøll T, Andersen HU, Bruun JM. The dietary education trial in carbohydrate counting (DIET-CARB Study): Study protocol for a randomised, parallel, open-label, intervention study comparing different approaches to dietary self-management in patients with Type 1 diabetes. BMJ Open. 2019; 9(9):e029859. [DOI:10.1136/bmjopen-2019-029859] [PMID] [PMCID]
- Snyder LL, Stafford JM, Dabelea D, Divers J, Imperatore G, Law J, et al. Socio-economic, demographic, and clinical correlates of poor glycaemic control within insulin regimens among children with Type 1 diabetes: The SEARCH for Diabetes in Youth Study. Diabetic Medicine. 2019; 36(8):1028-36. [DOI:10.1111/dme.13983] [PMID] [PMCID]
- No Authors. Invited abstracts. Pediatric Diabetes. 2017; 18(S25):4-17. [DOI:10.1111/pedi.12586] [PMID]
Article Type : Applicable |
Subject:
Special
Received: 2021/03/1 | Accepted: 2021/03/20 | Published: 2021/03/20
Received: 2021/03/1 | Accepted: 2021/03/20 | Published: 2021/03/20
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





.jpg)
