Thu, Apr 25, 2024
Volume 31, Issue 1 (12-2021)
JHNM 2021, 31(1): 26-34 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ranjbar M, Masoudnia E, Haghshenas Mojaver M. A Comparative Study on Psychosocial Factors between Mothers of Infants with and without Physical Abnormalities. JHNM 2021; 31 (1) :26-34
URL: http://hnmj.gums.ac.ir/article-1-1532-en.html
URL: http://hnmj.gums.ac.ir/article-1-1532-en.html
1- Sociology (MSA), School of Literature & Humanity, University of Guilan, Rasht, Iran
2- Associate Professor, Department of Social Sciences, School of Literature & Humanity, University of Guilan, Rasht, Iran , masoudnia@guilan.ac.ir
3- Assistant Professor, Babol University of Medical Sciences, Babol, Iran
2- Associate Professor, Department of Social Sciences, School of Literature & Humanity, University of Guilan, Rasht, Iran , masoudnia@guilan.ac.ir
3- Assistant Professor, Babol University of Medical Sciences, Babol, Iran
Full-Text [PDF 565 kb]
(653 Downloads)
| Abstract (HTML) (1683 Views)
Full-Text: (505 Views)
Introduction
ongenital anomalies are one of the most important causes of disability and mortality in childhood whose hospitalization costs and therapeutic interventions put heavy burden on the health system and familis [1]. They are a diverse group of disorders with prenatal origin that can be caused by single gene defects, chromosomal abnormalities, maternal infections and maternal diseases during pregnancy, such as diabetes mellitus, iodine and folic acid deficiency, abuse of alcohol, medications or recreational drugs (e.g. cigarette), exposure to certain environmental chemicals and radiation [2].
The incidence of congenital anomalies may vary based on time and place. It occurs by the complicated interaction of known and unknown genetic and environmental factors, including social, cultural, and ethnic. According to the World Health Organization (WHO), more than 8 million babies worldwide are born each year with a serious birth defect. Birth defects are a leading cause of infant death, and babies who survive may be physically or mentally disabled and put a costly burden on their families and communities [3]. The proportion of global neonatal mortality due to these defects increased from 3% in 2008 to 4.4% in 2013[4]. In Iran, the incidence of congenital anomalies is 10.1 per 1,000 live births in Gorgan city (northern Iran) and 28 per 1000 live births in Yazd city (southern Iran) [5]. A study by Aramesh et al. reported that, out of 1,620 newborns in Ahwaz city in 2011, 284 died; 79.9% of them were premature babies, 77.1% had weights< 2500 gr, and 78.2% died in the first week after birth. The most common causes of mortality were prematurity, congenital anomalies, birth defects, infections and other causes [6].
Various studies have been conducted in Iran on congenital anomalies and their etiology [7, 8, 9, 10, 11, 12], but few studies have examined the relationship between psychosocial factors and birth defects. In a study, Ghavi et al. [13] found a significant relationship between maternal lifestyle during pregnancy and low birth weight after delivery. Alhusen [14] in a study on the maternal-fetal attachment and its effect on the health of infant at birth showed that anxiety causes mother’s inappropriate responses to the fetus and reduces maternal-fetal attachment. As a result, mothers who have less attachment to their fetus have more anxiety and depression, which can lead to adverse effects in pregnancy.
Basharpour et al. [15] found that health beliefs and health promoting behaviors, especially physical activity and stress management, are associated with anxiety during pregnancy. However, the role of social-psychological factors has been neglected in these studies. In this regard, the present study aimed to determine the difference between mothers of infants with and without physical abnormalities in terms of psychosocial factors such as lifestyle, social support, mental health, coping strategies, and perceived stress intensity.
Materials and Methods
This is a case-control study. The study population consists of all mothers referred to health centers in Amol, Iran for postnatal care in 2018. Of these, 266 mothers were selected using a convenience sampling method and divided into two groups including mothers of infants with physical abnormalities (case group, n=133) and mothers of healthy infants (control group, n=133). The sample size for the case group was determined using Cochran’s formula, and for the control group by using homogenization method. To assess the birth defects in infants, a pre-test was performed on 60 mothers (30 with and 30 without physically-abnormal infants).
In calculating sample size, since the physical abnormality was a qualitative variable and there was a lack of access to the proportion of mothers having children with birth defects, the estimated proportion of population was set as P=0.5, and the confidence interval and the estimation error were considered 0.95% and 5%, respectively. Moreover, the amount of negligible error in estimation was considered 0.06. The inclusion criteria for the case group were: apparent physical defect and abnormal height (<40 cm), weight (<2500 gr), and head circumference (<32 cm) in the infants. The inclusion criteria for control group were normal height, weight, and head circumference, and no apparent physical defect in the infants.
The data were collected by:
A. A demographic form; surveying age, infant gender, education, income, job, place of residence, history of alcohol use and smoking, history of symptoms during pregnancy such as rubella, toxoplasmosis, cytomegalovirus and chickenpox.
B. Health-Promoting Lifestyle Profile (HPLP) [16] containing 52 items rated on a 4-point Likert scale (never, sometimes, often, and routinely) and measures health promoting behaviors under 6 dimensions: nutrition (having a dietary pattern and food choices, with 8 items), physical activity (following exercise, with 8 items), health responsibility (13 items), stress management (identifying stress resources and stress management measures, with 5 items), interpersonal relations (having intimate relationships to others, with 8 items), and spiritual growth (feeling purposefulness and satisfied with individual progress awareness, with 10 items). This questionnaire was translated to Persian by Mohammadi Zeidi et al. [17].
C. Multidimensional Scale of Perceived Social Support (MSPSS) [18] containing 12 items rated on a 5-point Likert-type scale (from strongly disagree to strongly agree), measures the perceived social support from friends (4 items), family (4 items), and significant others such as teacher or counselor (4 items). The validity of the Persian version of this questionnaire was confirmed using factor analysis by Masoudnia [19].
D. Coping Strategies Scale - Short Form (CSS-SF) [20] consisted of 17 items rated on a 5-point Likert scale (very high, high, moderate, low, and very low), measures the coping strategies in two areas: problem-focused (seeking social support, problem-based coping, and active coping) and emotion-focused (positive reappraisal/adaptation, escape avoidance, emotional-based coping, and self-control). The CSS-SF was translated to Persian by Masoudnia [21] and its satisfactory validity and reliability were reported.
E. Prenatal Distress Questionnaire (PDQ) [22], with 12 items rated on a 5-point Likert scale (strongly disagree, disagree, moderate, agree, strongly agree), measures the severity of perceived stress during pregnancy in 3 dimensions: concerns about the delivery and the health of the baby, concerns about the body weight/image, and concerns about emotions and relationships. A higher score indicates higher stress intensity. The Persian version of PDQ has also a good concurrent validity, test-retest stability, and internal consistency [23].
F. Goldberg and Hillier’s General Health Questionnaire–Short Form (GHQ-SF) [24], with 12 items rated on a 5-point Likert scale (I agree, I strongly agree, I do not mind, I disagree, I strongly disagree), measures mental problems under 4 dimensions: physical symptoms (3 items), anxiety/ insomnia (3 items), social dysfunction (3 items), and severe depression (3 items). Its lower score indicates better general health. The reliability and validity of the Persian version of GHQ-SF have been reported acceptable [25].
Information was given to the mothers about the study objectives and informed written consent was then obtained from them. Data were analyzed in SPSS v.20 software using descriptive statistics, Chi-square test and Independent t-test.
Results
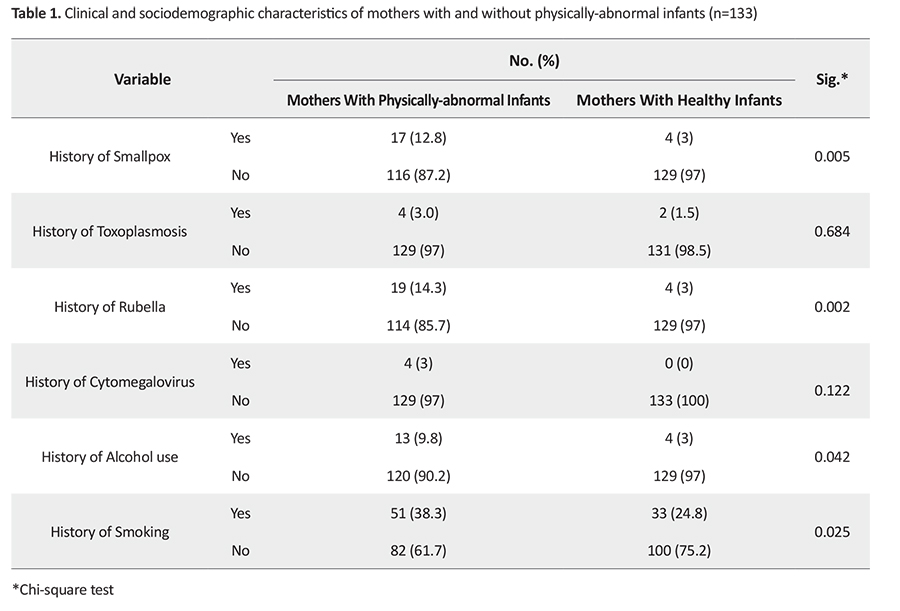
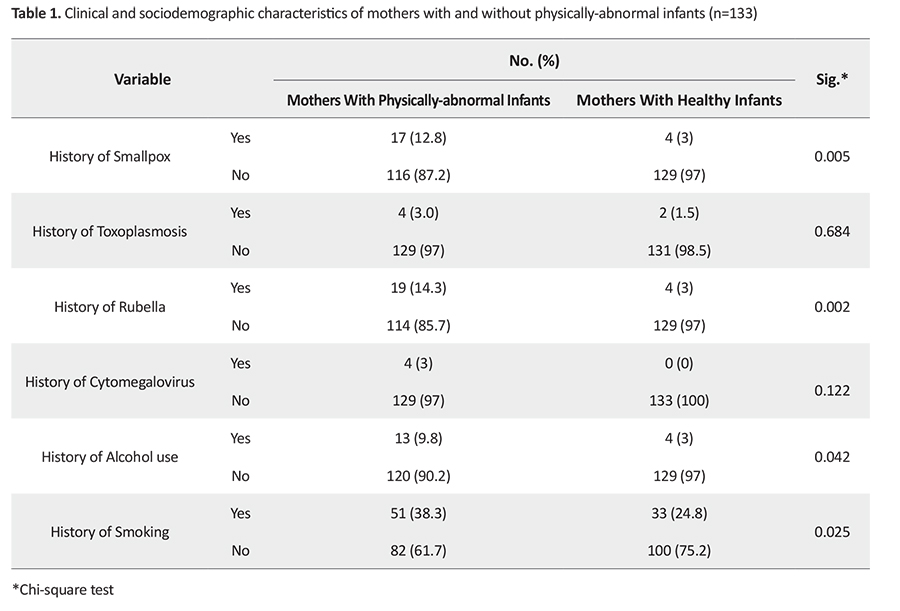
The mean age of mothers was 31.9±5.6 years. The prevalence of smoking and alcohol consumption in mothers of infants with physical abnormalities was higher than in mothers with healthy infants (Table 1).
There was a significant difference between the two groups of mothers in terms of lifestyle (P=0.003). The mean HPLP score of mothers without abnormal infants was higher than that of mothers with healthy infants (Table 2).

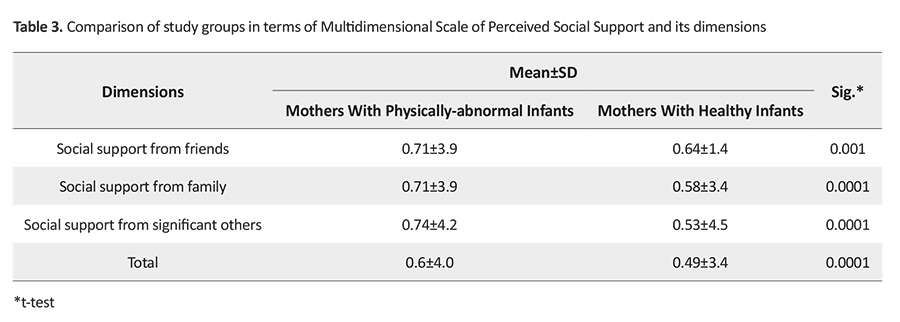
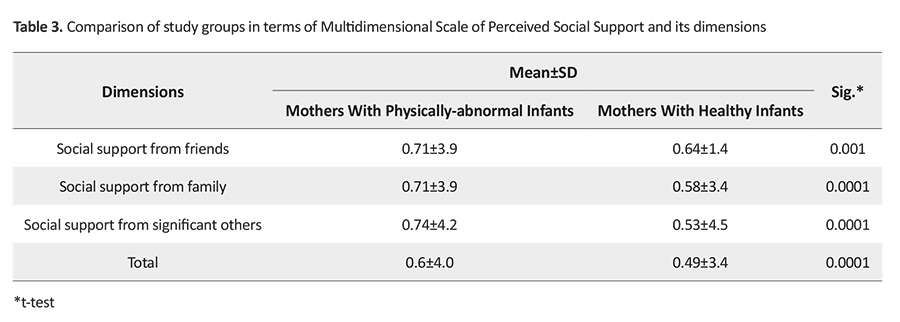
There was a significant difference between the two groups in terms of overall MSPSS) score (P=0.01), and its dimensions including the support from friends (P=0.01), family (P=0.01), and significant others (P=0.01) (Table 3).
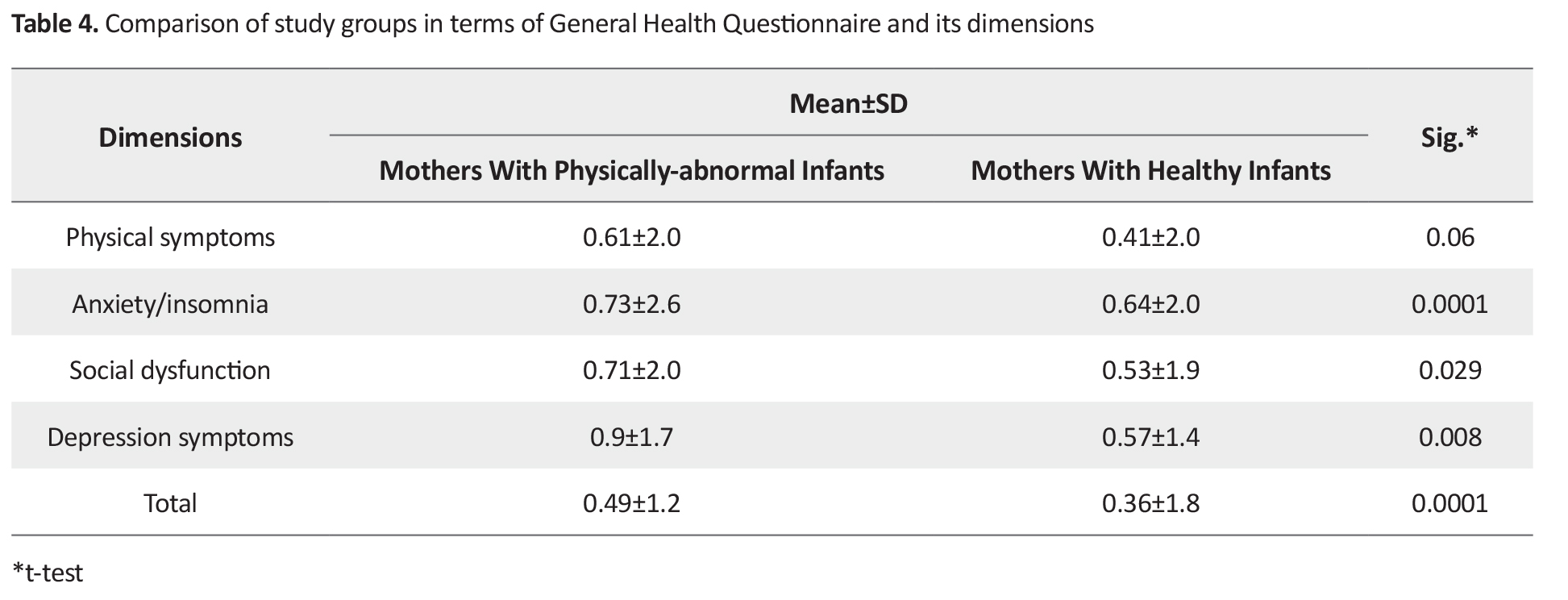
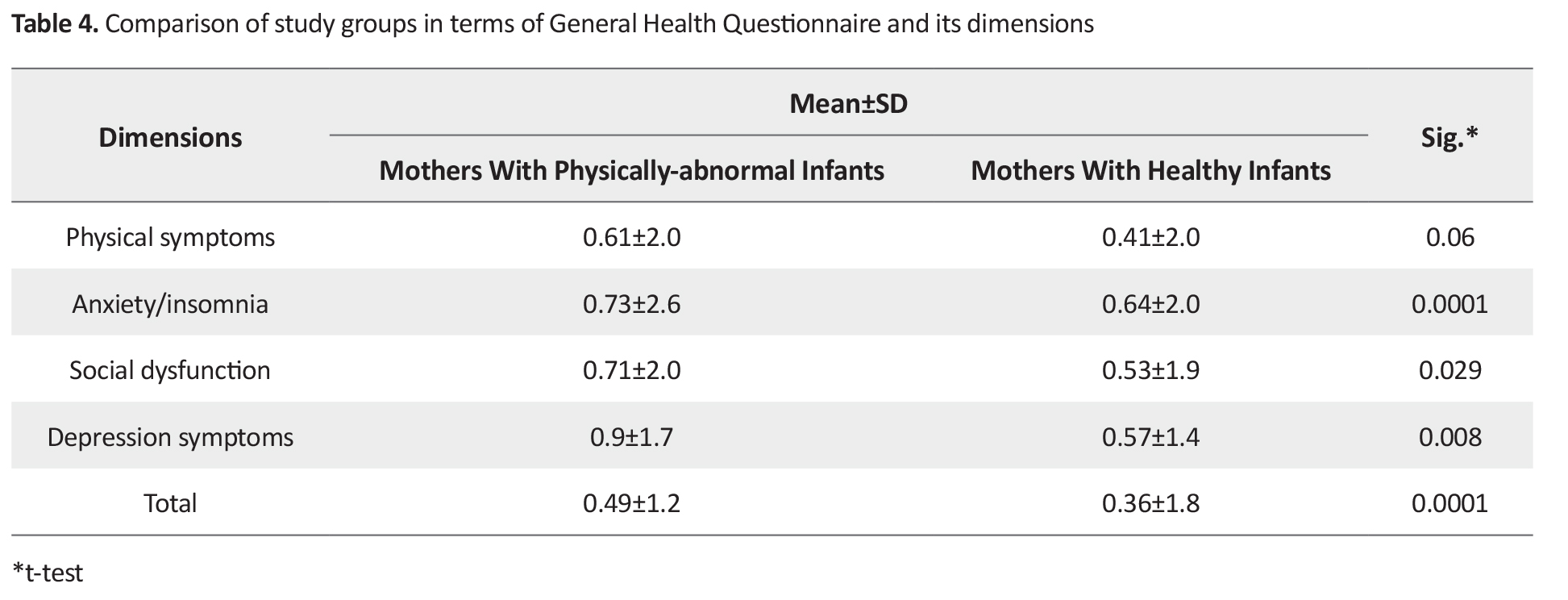
Comparison of mothers in terms of GHQ-SF score showed a significant difference between them (P=0.0001) (Table 4).
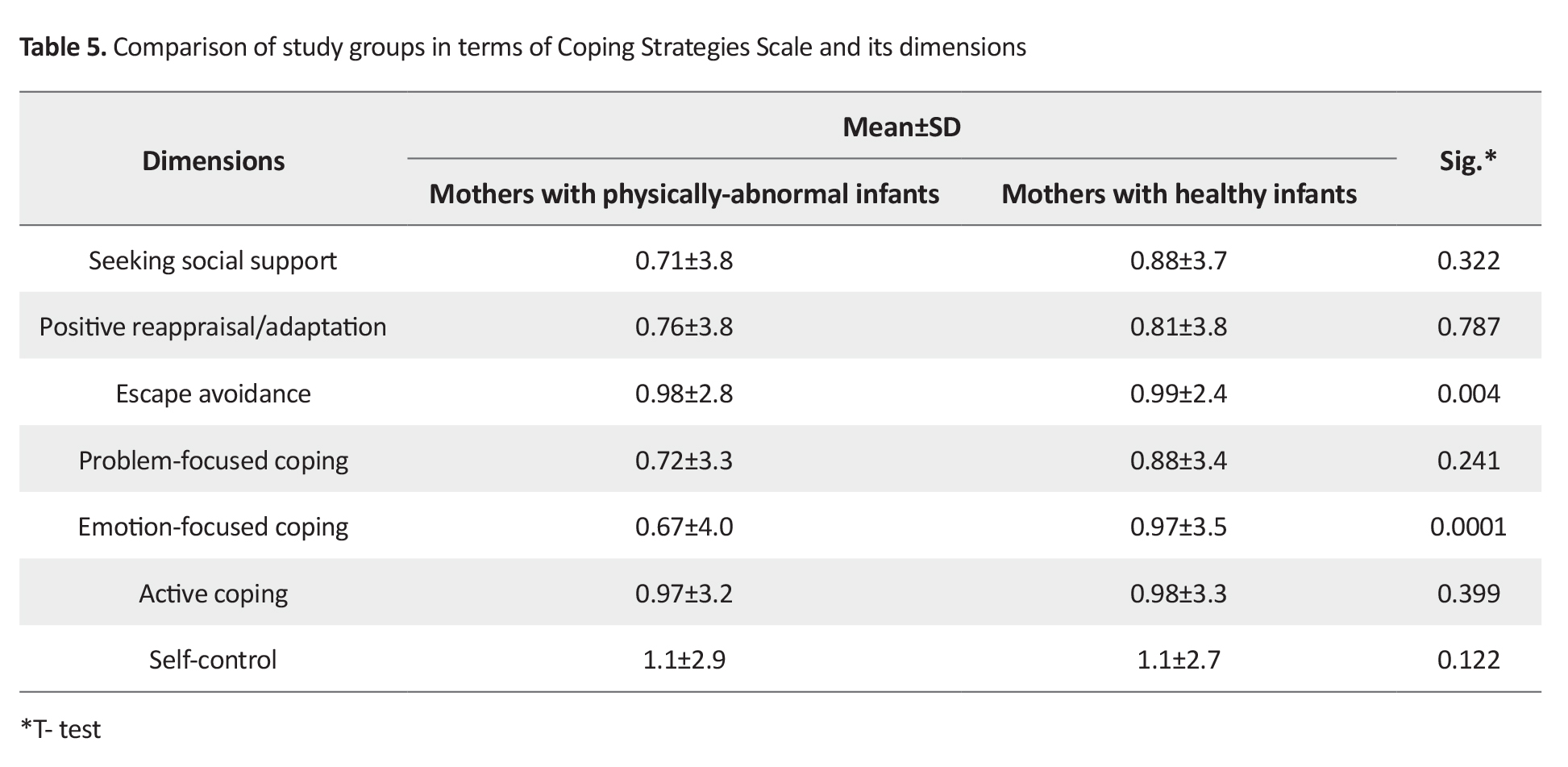
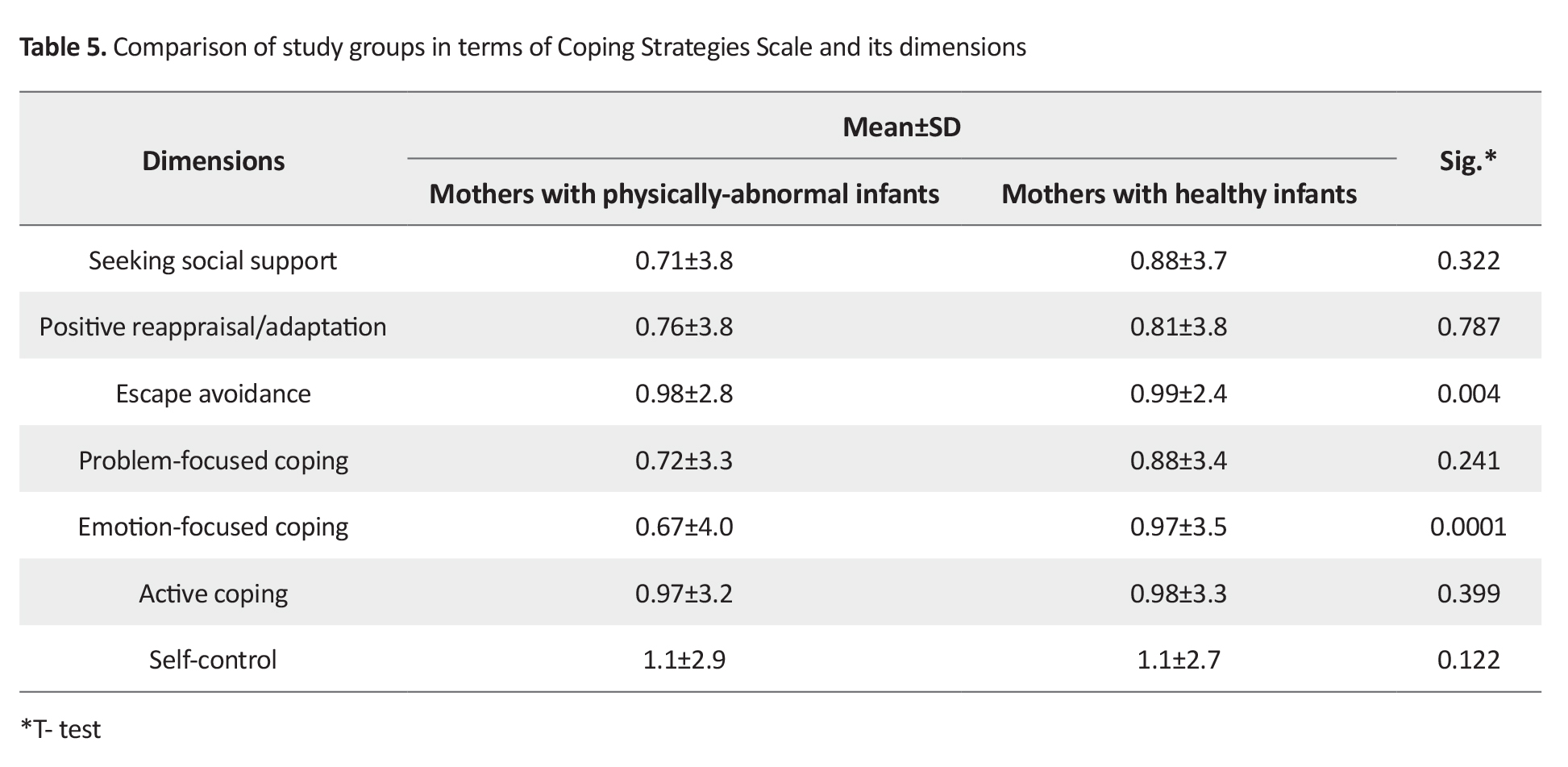
Moreover, there was a significant difference between the two groups of mothers in terms of CSS dimensions of escape avoidance (P=0.004) and emotion-focused (P=0.0001) strategies (Table 5).
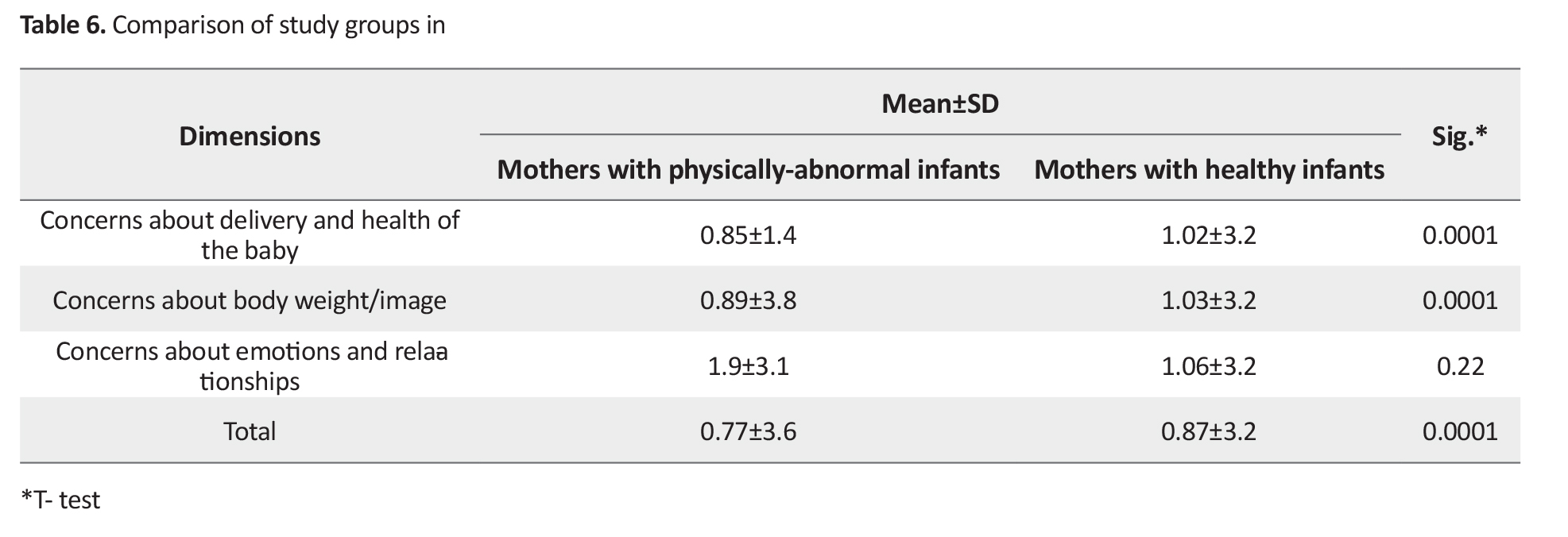
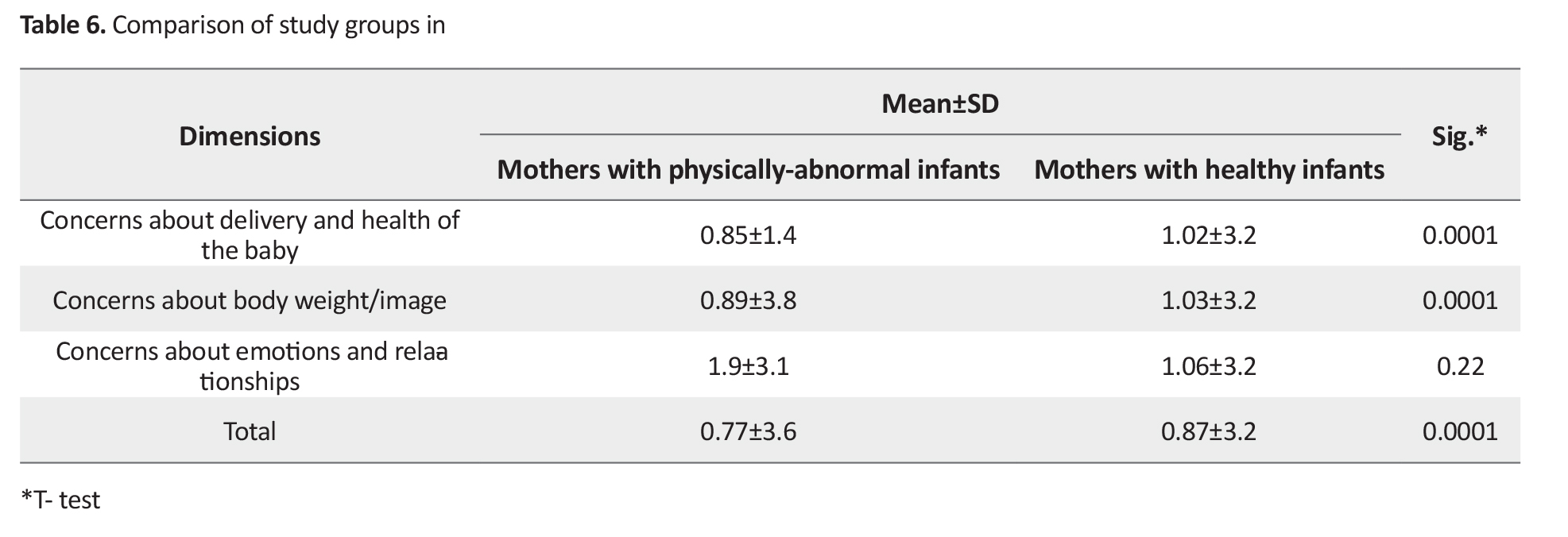
In terms of PDQ, the comparison showed significant difference between the two groups in terms of overall PDQ score (P=0.0001) (Table 6).
Discussion
The aim of this study was to evaluate the difference between mothers with and without physically-abnormal infants in terms of psychosocial factors. The prevalence of smoking and alcohol use during pregnancy was higher in mothers of infants with physical abnormalities than in mothers with healthy infants. Some studies have shown that maternal smoking during pregnancy is an established risk factor for miscarriage/perinatal mortality, low birthweight, premature births and small fetuses, and increases the likelihood of fetal abnormality [26, 27]. The frequency of smallpox and rubella in mothers who had newborns with physical abnormalities were higher than in those with healthy baby. This finding is in line with the findings of Joshaghan [28].
Regarding HPLP dimensions, There was a significant difference between mothers with and without physically-abnormal infants in terms of spiritual growth. Mothers with healthy newborns had more hope, satisfaction, and purposefulness in their lives than mothers with physically-abnormal infants. This result is consistent with the results of Avaznejad et al. [29]. Mothers with healthy babies emphasized on the positive aspects of their empowerment in different areas of life, which makes them more resistant to difficult conditions, but such conditions are also observed in mothers of infants with physical abnormalities.
There was no difference between mothers with and without physically-abnormal infants in terms of the health responsibility, as other component of HPLP. However, Jamshidi Manesh [30] reported that mothers who had higher level of health-responsibility had healthier babies. This discrepancy may be due to the use of different measurement instruments. Regarding other dimensions of HPLP, mothers in both groups had satisfying interpersonal relationships and could solve their problems through dialogue. These results are consistent with the results of Ghavi et al.'s study [13].
In terms of stress management dimension, there was also a significant difference between the two groups, where mothers with healthy baby had a greater degree of relaxation. This result is consistent with the results of other studies [31, 32]. Mothers with healthy infants had more physical activity than mothers with physically-abnormal infants. Hajikazemi et al. [33] showed that exercise during pregnancy increases birth weight, shortens the delivery stages and reduces the need for delivery through cesarean section; it is an important contribution to normal delivery. In terms of the dimension of nutrition, mothers with healthy newborns had better dietary pattern compared to mothers with physically-abnormal infants.
Poor nutrition during pregnancy is associated with irreversible damage to the infant brain and central nervous system, leading to poor brain development and intelligence. This finding is similar to that of Kaiserl and Allen [34]. It seems that economic, social and cultural factors make it difficult for many women in developing countries, including Iran, to have proper nutrition and health care. Health may be an important determinant of opportunities in life and this process termed “selection by health”, and suggest that health selects people in different social strata [35].
The present study revealed the relationship between inadequate perceived social support of mothers during pregnancy and the incidence of physical abnormalities in newborns. The overall MSPSS score of mothers with healthy baby was lower than that of mothers with physically-abnormal infants. Bradley and Cartwright [36] showed that mothers who had received support from friends during pregnancy and had less interpersonal conflicts reported better coping strategies. This result of our study is consistent with the results of Abdollahpour et al. [37]. The level of perceived social support from significant others in mothers with physically-abnormal infants was lower than that of mothers with healthy infants. Social support from relatives during pregnancy and after birth is important for women [38]. Social support theories show that social support contributes to the control of maternal stress and distress during pregnancy. It helps moderate the neurological effects and acute/chronic stress in mothers during pregnancy, and regulate the stressful conditions of pregnancy [39].
There was a significant difference between mothers with and without physically-abnormal infants in all GHQ components except in physical symptoms. This result is consistent with the results of Foruzandeh et al. [40]. The symptoms of anxiety and insomnia in mothers with physically-abnormal infants were higher than in mothers with healthy infants. This result is consistent with the results of Green et al. [41]. Mothers with physically-abnormal newborns also showed more symptoms of social dysfunction during pregnancy. According to studies, the feeling of isolation and reduced social activity in mothers, weaken their social function and cause psychological problems during pregnancy [42]. There was also a significant difference between the two groups of mothers in terms of depression symptoms during pregnancy. This result is consistent with the findings of some studies [43, 44]. In general, it seems that women with low general health have higher tendency to use alcohol and drugs during pregnancy, and lower willingness to receive proper care during pregnancy.
Another variable whose relationship with birth defects was investigated was coping strategy. Coping strategies in this study were categorized into two general categories of problem-focused and emotional-focused strategies based on Lazaru and Folkman’s theory of coping [45]. The results showed that, although the mean score of problem-focused coping strategies in mothers with healthy infants was higher than in mothers with physically-abnormal infants, the difference between them was not statistically significant. Regarding emotional-focused coping strategies, mothers with physically-abnormal infants avoided confronting stressful conditions, resolved them during pregnancy, and tended to use an emotion-focused coping strategy more than mothers with healthy infants. They expressed their feelings such as fear, anger, and discomfort during pregnancy more than mothers with healthy infants. According to Lazarus and Folkman [45], when a mother adopts an emotion-focused strategy, she tries to control stressors by methods such as telling a trusted friend or a family member about her feelings. This strategy makes it possible to ignore stressors rather than solving problems.
Our study showed that mothers with physically-abnormal infants had more concerns about their body weight and image during pregnancy than mothers with healthy babies. Negahban et al. [46] showed that the most common cause of concern during pregnancy is the fear of pain and fetal harm. In addition, the risk of low birth weight in distressed mothers is higher than in other mothers [47]. Body dissatisfaction can have direct or indirect effects on maternal and fetal health such as depression, the use of unhealthy ways to lose weight, low birth weight, premature birth, and developmental delay.
There were some limitations in conducting this study. We used a self-report tool and, hence, it is possible that the mothers’ perceptions have not been correctly reported. Therefore, future studies are recommended to use other measurement methods along the tool that indirectly measure variables. The second limitation was related to the culture. Since the behavior and interaction of mothers are shaped by cultural patterns and the behavioral and cultural patterns of mothers living in northern Iran are different compared to those living in other parts, the results can not be generalized to other parts of the country. Therefore, it is recommended that more studies be conducted in other cities in order to obtain more accurate results on the effect of psychosocial factors on birth defects.
Ethical Considerations
Compliance with ethical guidelines
This study was extracted from a master thesis. All ethical principles were met in this study. Prior to study, the participants were informed about the study objectives and then a written informed consent was obtained from them.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-profit sectors.
Authors contributions
Conceptualization, editing & review: All authors; initial draft preparation, investigation, and data analysis: Ebrahim Masoudnia, Mahtab Ranjbar.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgements
The authors would like to thank the personnel of Fatemeh Al-Zahra and Sotte Kola health centers, Department of Obstetrics and Gynecology, Imam Ali Hospital in Amol city, and the participants for their cooperation.
References
ongenital anomalies are one of the most important causes of disability and mortality in childhood whose hospitalization costs and therapeutic interventions put heavy burden on the health system and familis [1]. They are a diverse group of disorders with prenatal origin that can be caused by single gene defects, chromosomal abnormalities, maternal infections and maternal diseases during pregnancy, such as diabetes mellitus, iodine and folic acid deficiency, abuse of alcohol, medications or recreational drugs (e.g. cigarette), exposure to certain environmental chemicals and radiation [2].
The incidence of congenital anomalies may vary based on time and place. It occurs by the complicated interaction of known and unknown genetic and environmental factors, including social, cultural, and ethnic. According to the World Health Organization (WHO), more than 8 million babies worldwide are born each year with a serious birth defect. Birth defects are a leading cause of infant death, and babies who survive may be physically or mentally disabled and put a costly burden on their families and communities [3]. The proportion of global neonatal mortality due to these defects increased from 3% in 2008 to 4.4% in 2013[4]. In Iran, the incidence of congenital anomalies is 10.1 per 1,000 live births in Gorgan city (northern Iran) and 28 per 1000 live births in Yazd city (southern Iran) [5]. A study by Aramesh et al. reported that, out of 1,620 newborns in Ahwaz city in 2011, 284 died; 79.9% of them were premature babies, 77.1% had weights< 2500 gr, and 78.2% died in the first week after birth. The most common causes of mortality were prematurity, congenital anomalies, birth defects, infections and other causes [6].
Various studies have been conducted in Iran on congenital anomalies and their etiology [7, 8, 9, 10, 11, 12], but few studies have examined the relationship between psychosocial factors and birth defects. In a study, Ghavi et al. [13] found a significant relationship between maternal lifestyle during pregnancy and low birth weight after delivery. Alhusen [14] in a study on the maternal-fetal attachment and its effect on the health of infant at birth showed that anxiety causes mother’s inappropriate responses to the fetus and reduces maternal-fetal attachment. As a result, mothers who have less attachment to their fetus have more anxiety and depression, which can lead to adverse effects in pregnancy.
Basharpour et al. [15] found that health beliefs and health promoting behaviors, especially physical activity and stress management, are associated with anxiety during pregnancy. However, the role of social-psychological factors has been neglected in these studies. In this regard, the present study aimed to determine the difference between mothers of infants with and without physical abnormalities in terms of psychosocial factors such as lifestyle, social support, mental health, coping strategies, and perceived stress intensity.
Materials and Methods
This is a case-control study. The study population consists of all mothers referred to health centers in Amol, Iran for postnatal care in 2018. Of these, 266 mothers were selected using a convenience sampling method and divided into two groups including mothers of infants with physical abnormalities (case group, n=133) and mothers of healthy infants (control group, n=133). The sample size for the case group was determined using Cochran’s formula, and for the control group by using homogenization method. To assess the birth defects in infants, a pre-test was performed on 60 mothers (30 with and 30 without physically-abnormal infants).
In calculating sample size, since the physical abnormality was a qualitative variable and there was a lack of access to the proportion of mothers having children with birth defects, the estimated proportion of population was set as P=0.5, and the confidence interval and the estimation error were considered 0.95% and 5%, respectively. Moreover, the amount of negligible error in estimation was considered 0.06. The inclusion criteria for the case group were: apparent physical defect and abnormal height (<40 cm), weight (<2500 gr), and head circumference (<32 cm) in the infants. The inclusion criteria for control group were normal height, weight, and head circumference, and no apparent physical defect in the infants.
The data were collected by:
A. A demographic form; surveying age, infant gender, education, income, job, place of residence, history of alcohol use and smoking, history of symptoms during pregnancy such as rubella, toxoplasmosis, cytomegalovirus and chickenpox.
B. Health-Promoting Lifestyle Profile (HPLP) [16] containing 52 items rated on a 4-point Likert scale (never, sometimes, often, and routinely) and measures health promoting behaviors under 6 dimensions: nutrition (having a dietary pattern and food choices, with 8 items), physical activity (following exercise, with 8 items), health responsibility (13 items), stress management (identifying stress resources and stress management measures, with 5 items), interpersonal relations (having intimate relationships to others, with 8 items), and spiritual growth (feeling purposefulness and satisfied with individual progress awareness, with 10 items). This questionnaire was translated to Persian by Mohammadi Zeidi et al. [17].
C. Multidimensional Scale of Perceived Social Support (MSPSS) [18] containing 12 items rated on a 5-point Likert-type scale (from strongly disagree to strongly agree), measures the perceived social support from friends (4 items), family (4 items), and significant others such as teacher or counselor (4 items). The validity of the Persian version of this questionnaire was confirmed using factor analysis by Masoudnia [19].
D. Coping Strategies Scale - Short Form (CSS-SF) [20] consisted of 17 items rated on a 5-point Likert scale (very high, high, moderate, low, and very low), measures the coping strategies in two areas: problem-focused (seeking social support, problem-based coping, and active coping) and emotion-focused (positive reappraisal/adaptation, escape avoidance, emotional-based coping, and self-control). The CSS-SF was translated to Persian by Masoudnia [21] and its satisfactory validity and reliability were reported.
E. Prenatal Distress Questionnaire (PDQ) [22], with 12 items rated on a 5-point Likert scale (strongly disagree, disagree, moderate, agree, strongly agree), measures the severity of perceived stress during pregnancy in 3 dimensions: concerns about the delivery and the health of the baby, concerns about the body weight/image, and concerns about emotions and relationships. A higher score indicates higher stress intensity. The Persian version of PDQ has also a good concurrent validity, test-retest stability, and internal consistency [23].
F. Goldberg and Hillier’s General Health Questionnaire–Short Form (GHQ-SF) [24], with 12 items rated on a 5-point Likert scale (I agree, I strongly agree, I do not mind, I disagree, I strongly disagree), measures mental problems under 4 dimensions: physical symptoms (3 items), anxiety/ insomnia (3 items), social dysfunction (3 items), and severe depression (3 items). Its lower score indicates better general health. The reliability and validity of the Persian version of GHQ-SF have been reported acceptable [25].
Information was given to the mothers about the study objectives and informed written consent was then obtained from them. Data were analyzed in SPSS v.20 software using descriptive statistics, Chi-square test and Independent t-test.
Results
The mean age of mothers was 31.9±5.6 years. The prevalence of smoking and alcohol consumption in mothers of infants with physical abnormalities was higher than in mothers with healthy infants (Table 1).
There was a significant difference between the two groups of mothers in terms of lifestyle (P=0.003). The mean HPLP score of mothers without abnormal infants was higher than that of mothers with healthy infants (Table 2).

There was a significant difference between the two groups in terms of overall MSPSS) score (P=0.01), and its dimensions including the support from friends (P=0.01), family (P=0.01), and significant others (P=0.01) (Table 3).
Comparison of mothers in terms of GHQ-SF score showed a significant difference between them (P=0.0001) (Table 4).
Moreover, there was a significant difference between the two groups of mothers in terms of CSS dimensions of escape avoidance (P=0.004) and emotion-focused (P=0.0001) strategies (Table 5).
In terms of PDQ, the comparison showed significant difference between the two groups in terms of overall PDQ score (P=0.0001) (Table 6).
Discussion
The aim of this study was to evaluate the difference between mothers with and without physically-abnormal infants in terms of psychosocial factors. The prevalence of smoking and alcohol use during pregnancy was higher in mothers of infants with physical abnormalities than in mothers with healthy infants. Some studies have shown that maternal smoking during pregnancy is an established risk factor for miscarriage/perinatal mortality, low birthweight, premature births and small fetuses, and increases the likelihood of fetal abnormality [26, 27]. The frequency of smallpox and rubella in mothers who had newborns with physical abnormalities were higher than in those with healthy baby. This finding is in line with the findings of Joshaghan [28].
Regarding HPLP dimensions, There was a significant difference between mothers with and without physically-abnormal infants in terms of spiritual growth. Mothers with healthy newborns had more hope, satisfaction, and purposefulness in their lives than mothers with physically-abnormal infants. This result is consistent with the results of Avaznejad et al. [29]. Mothers with healthy babies emphasized on the positive aspects of their empowerment in different areas of life, which makes them more resistant to difficult conditions, but such conditions are also observed in mothers of infants with physical abnormalities.
There was no difference between mothers with and without physically-abnormal infants in terms of the health responsibility, as other component of HPLP. However, Jamshidi Manesh [30] reported that mothers who had higher level of health-responsibility had healthier babies. This discrepancy may be due to the use of different measurement instruments. Regarding other dimensions of HPLP, mothers in both groups had satisfying interpersonal relationships and could solve their problems through dialogue. These results are consistent with the results of Ghavi et al.'s study [13].
In terms of stress management dimension, there was also a significant difference between the two groups, where mothers with healthy baby had a greater degree of relaxation. This result is consistent with the results of other studies [31, 32]. Mothers with healthy infants had more physical activity than mothers with physically-abnormal infants. Hajikazemi et al. [33] showed that exercise during pregnancy increases birth weight, shortens the delivery stages and reduces the need for delivery through cesarean section; it is an important contribution to normal delivery. In terms of the dimension of nutrition, mothers with healthy newborns had better dietary pattern compared to mothers with physically-abnormal infants.
Poor nutrition during pregnancy is associated with irreversible damage to the infant brain and central nervous system, leading to poor brain development and intelligence. This finding is similar to that of Kaiserl and Allen [34]. It seems that economic, social and cultural factors make it difficult for many women in developing countries, including Iran, to have proper nutrition and health care. Health may be an important determinant of opportunities in life and this process termed “selection by health”, and suggest that health selects people in different social strata [35].
The present study revealed the relationship between inadequate perceived social support of mothers during pregnancy and the incidence of physical abnormalities in newborns. The overall MSPSS score of mothers with healthy baby was lower than that of mothers with physically-abnormal infants. Bradley and Cartwright [36] showed that mothers who had received support from friends during pregnancy and had less interpersonal conflicts reported better coping strategies. This result of our study is consistent with the results of Abdollahpour et al. [37]. The level of perceived social support from significant others in mothers with physically-abnormal infants was lower than that of mothers with healthy infants. Social support from relatives during pregnancy and after birth is important for women [38]. Social support theories show that social support contributes to the control of maternal stress and distress during pregnancy. It helps moderate the neurological effects and acute/chronic stress in mothers during pregnancy, and regulate the stressful conditions of pregnancy [39].
There was a significant difference between mothers with and without physically-abnormal infants in all GHQ components except in physical symptoms. This result is consistent with the results of Foruzandeh et al. [40]. The symptoms of anxiety and insomnia in mothers with physically-abnormal infants were higher than in mothers with healthy infants. This result is consistent with the results of Green et al. [41]. Mothers with physically-abnormal newborns also showed more symptoms of social dysfunction during pregnancy. According to studies, the feeling of isolation and reduced social activity in mothers, weaken their social function and cause psychological problems during pregnancy [42]. There was also a significant difference between the two groups of mothers in terms of depression symptoms during pregnancy. This result is consistent with the findings of some studies [43, 44]. In general, it seems that women with low general health have higher tendency to use alcohol and drugs during pregnancy, and lower willingness to receive proper care during pregnancy.
Another variable whose relationship with birth defects was investigated was coping strategy. Coping strategies in this study were categorized into two general categories of problem-focused and emotional-focused strategies based on Lazaru and Folkman’s theory of coping [45]. The results showed that, although the mean score of problem-focused coping strategies in mothers with healthy infants was higher than in mothers with physically-abnormal infants, the difference between them was not statistically significant. Regarding emotional-focused coping strategies, mothers with physically-abnormal infants avoided confronting stressful conditions, resolved them during pregnancy, and tended to use an emotion-focused coping strategy more than mothers with healthy infants. They expressed their feelings such as fear, anger, and discomfort during pregnancy more than mothers with healthy infants. According to Lazarus and Folkman [45], when a mother adopts an emotion-focused strategy, she tries to control stressors by methods such as telling a trusted friend or a family member about her feelings. This strategy makes it possible to ignore stressors rather than solving problems.
Our study showed that mothers with physically-abnormal infants had more concerns about their body weight and image during pregnancy than mothers with healthy babies. Negahban et al. [46] showed that the most common cause of concern during pregnancy is the fear of pain and fetal harm. In addition, the risk of low birth weight in distressed mothers is higher than in other mothers [47]. Body dissatisfaction can have direct or indirect effects on maternal and fetal health such as depression, the use of unhealthy ways to lose weight, low birth weight, premature birth, and developmental delay.
There were some limitations in conducting this study. We used a self-report tool and, hence, it is possible that the mothers’ perceptions have not been correctly reported. Therefore, future studies are recommended to use other measurement methods along the tool that indirectly measure variables. The second limitation was related to the culture. Since the behavior and interaction of mothers are shaped by cultural patterns and the behavioral and cultural patterns of mothers living in northern Iran are different compared to those living in other parts, the results can not be generalized to other parts of the country. Therefore, it is recommended that more studies be conducted in other cities in order to obtain more accurate results on the effect of psychosocial factors on birth defects.
Ethical Considerations
Compliance with ethical guidelines
This study was extracted from a master thesis. All ethical principles were met in this study. Prior to study, the participants were informed about the study objectives and then a written informed consent was obtained from them.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-profit sectors.
Authors contributions
Conceptualization, editing & review: All authors; initial draft preparation, investigation, and data analysis: Ebrahim Masoudnia, Mahtab Ranjbar.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgements
The authors would like to thank the personnel of Fatemeh Al-Zahra and Sotte Kola health centers, Department of Obstetrics and Gynecology, Imam Ali Hospital in Amol city, and the participants for their cooperation.
References
- Shawky RM, Sadik DI. Congenital malformations prevalent among egyption children and associated risk factors. Egyptian Journal of Medical Human Genetics. 2011; 12(1):69-78. [DOI:10.1016/j.ejmhg.2011.02.016]
- Koumi MA, Banna EA, Lebda I. Pattern of congenital anomalies in newborn: A hospital-based study. Pediatric Reports. 2013; 5(1):20-3. [DOI:10.4081%2Fpr.2013.e5] [PMID][PMCID]
- World Health Organization (WHO). World birth defects. https://www.who.int/life-course/news/events/world-birth-defects-day-2018/en/
- Oestergaard MZ, Inoue M, Yoshida S, Mahanani WR, Gore FM, Cousens S, et al. Neonatal mortality levels for 193 countries in 2009 with trends since 1990: A systematic analysis of Progress, projections, and priorities. PLOS Medicine. 2011; 8(8):1-13. [DOI:10.1371/journal.pmed.1001080] [PMID] [PMCID]
- Golalipour MJ, Mirfazeli A, Mobasheri E. [Incidence and pattern of congenital malformations in Gorgan-north of Iran (Persian)]. Journal of Medical Sciences. 2013; 13(8):834-8. [DOI:10.3923/jms.2013.834.838]
- Aramesh MR, Malekian A, Dehdashtian M, Shahori A, Monjezi L. [Determination of neonatal mortality causes among neonates admitted in NICU at Imam Khomeini Hospital, Ahwaz, 2011-2012 (Persian)]. Razi Journal of Medical Sciences. 2014; 21(120):36-43. http://rjms.iums.ac.ir/article-1-3141-en.html
- Lorente C, Cordier S, Goujard J, Aymé S, Bianchi F, Calzolari E, et al. Tobacco and alcohol use during pregnancy and risk of oral clefts. Occupational Exposure and Congenital Malformation Working Group. American Journal of Public Health. 2000; 90(3):415-9. [DOI:10.2105/AJPH.90.3.415] [PMID] [PMCID]
- Rajabian MH, Aghaei S. Cleft lip and palate in southwestern Iran: An epidemiologic study of live births. Annals of Saudi Medicine. 2005; 25(5):385-8. [DOI:10.5144/0256-4947.2005.385] [PMID] [PMCID]
- Eftekhar T, Ghanbari Z, Haghollahi F. [Neural tube defect in alive neonates: Incidence rate and predisposing factors (Persian)]. Tehran University Medical Journal. 2008; 66(3):191-5. http://tumj.tums.ac.ir/article-1-623-fa.html
- Azadi M, Naji T. [Evaluation of types and incidence of congenital abnormalities in newborns (Persian)]. Journal of Laboratory Diagnosis. 2016; 124:40-2. magiran.com/p1542727
- Hesami M, Ghafarpasand F, Nikouee F. [Prevalence rate of congenital anomaly of male newborn in Fasa Hospital (Persian)]. Journal of Fasa University of Medical Sciences. 2011; 1(3):149-53. http://journal.fums.ac.ir/article-1-79-fa.html
- Mesbah H. [A study of complications of clubfoot after turbo operation (Persian)]. Medical Journal Of Tabriz University Of Medical Sciences. 2001; 35(51):79-82. Available at: https://majalleh.tbzmed.ac.ir/
- Ghavi A, Fadakar Sogheh K, Niknami M, Kazem Nejad H. [Investigating the relationship between maternal lifestyle during pregnancy and low-birth-weight of term neonates (Persian)]. Iranian Journal of Obstetrics, Gynecology and Infertility. 2012; 15(29):14-24. [DOI:10.22038/ijogi.2012.58]
- Alhusen JL. A literature update on maternal-fetal attachment. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2008; 37(3):315-28.[DOI:10.1111%2Fj.1552-6909.2008.00241.x] [PMID] [PMCID]
- Basharpoor S, Heydarirad H, Atadokht A, Daryadel SJ, Nasiri-Razi R. [The role of health beliefs and health promoting lifestyle in predicting pregnancy anxiety among pregnant women (Persian)]. Iranian Journal of Health Education and Health Promotion. 2015; 3(3):171-80. http://journal.ihepsa.ir/article-1-260-fa.html
- Walker SN, Sechrist KR, Pender NJ. The Health-Promoting Lifestyle Profile: Development and psychometric characteristics. Nursing Research. 1987; 36(2):76-81. [DOI:10.1097/00006199-198703000-00002] [PMID]
- Mohammadi Zeidi I, Pakpour Hajiagha A, Mohammadi Zeidi B. [Reliability and validity of persian version of the health-promoting lifestyle profile (Persian)]. Journal of Mazandaran University of Medical Sciences. 2012; 21(1):102-13. http://jmums.mazums.ac.ir/article-1-955-en.html
- Canty-Mitchell J, Zimet GD. Psychometric properties of the Multidimensional Scale of Perceived Social Support in urban adolescents. American Journal of Community Psychology. 2000; 28(3):391-400. [DOI:10.1023/A:1005109522457] [PMID]
- Masoudnia E. [Relationship between perceived social support and risk of postpartum depression disorder. Iran Journal of Nursing (Persian)]. 2011; 24(70):8-18. http://ijn.iums.ac.ir/article-1-981-en.html
- Holahan CJ, Moos RH. Life stress and health: Personality, coping and family support in stress resistance. Journal of Personality & Social Psychology. 1985; 49(3):739-47. [DOI:10.1037/0022-3514.49.3.739] [PMID]
- Masoudnia E. [Impacts of social class on the illness behavior of patients with rheumatoid arthritis (Persian)]. [phD thesis]. University of Isfahan. 2005, pp: 133-134.
- Alderdice F, Lynn F. Factor structure of the Prenatal Distress Questionnaire. Journal of Midwifery. 2011;27(4):553-9. [DOI:10.1016/j.midw.2010.05.003] [PMID]
- Yousefi R. [Psychometric properties of Persian version of Parental Distress Questionnaire (PDQ) (Persian)]. Journal of Urmia Nursing and Midwifery Faculty. 2015; 13(3):215-25. http://unmf.umsu.ac.ir/article-1-1885-en.html
- Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Journal of Psychological Medicine. 1979; 9(1):139-45. [DOI:10.1017/S0033291700021644] [PMID]
- Taghavi S. The Normalization of General Health Questionnaire for Shiraz University Students (GHQ-28). Clinical Psychology & Personality. 2008; 15(28):1-12.
- Royal College of Physicians. Effects of maternal active and passive smoking on fetal and reproductive health. In: Passive Smoking and Children. A report by the Tobacco Advisory Group of the Royal College of Physicians, Chapter 3, 40-76. Eds: Britton J, Edwards R. Royal College of Physicians 2010.
- Hackshaw A, Rodeck C, Boniface S. Maternal smoking in pregnancy and birth defects: A systematic review based on 173 687 malformed cases and 11.7 million controls. Human Reproduction Update. 2011; 17(5):589-604. [DOI:10.1093/humupd/dmr022] [PMID] [PMCID]
- Joshaghan A, Ahmadi S, Motevalizadeh S, Zakiani S. [A review of the diagnosis of viral embryos before and after birth (Persian)]. Journal of Shahid Sadoughi University of Medical Sciences. 2008; 16(3):77-87. http://jssu.ssu.ac.ir/article-1-582-fa.html
- Avaznejad N, ravanipour M, bahreyni M, motamed N. [Comparison of spiritual health in mothers with healthy children and mothers of children with chronic disease in Kerman 2015-2016 (Persian)]. Nursing Journal of The Vulnerable. 2016; 3(8):13-25. http://njv.bpums.ac.ir/article-1-736-en.html
- Jamshidi Manesh M, Astaraki L, Behboodi Moghadam Z, Taghizadeh Z, Haghani H. [Maternal-fetal attachment and its associated factors (Persian)]. Hayat. 2013; 18(5):33-45. http://hayat.tums.ac.ir/article-1-4-en.html
- Shayeghian Z, RasolZade Tabatabae SK , Sedighi Louye E. [Effect of maternal anxiety during final 3 mounths period of pregnancy on labor process and neonatal health (Persian)]. Hayat. 2009; 14(3 & 4):57-64. http://hayat.tums.ac.ir/article-1-137-en.html
- Gennaro S, Hennessy MD. Psychological and physiological stress: Impact on preterm birth. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2003; 32(5):668-75. [DOI:10.1177/0884217503257484] [PMID]
- Hajikazemi ES, Heydari M, Feizi Z, Haghani H. [Effect of physical exercise on pregnancy outcome (Persian)]. Iran Journal of Nursing. 2001; 13(25):15-22. http://ijn.iums.ac.ir/article-1-247-en.html
- Kaiser l, Allen LH. Position of American dietetic association: Nutrition and lifestyle for a healthy pregnancy outcome. Journal of the American Dietetic Association. 2008; (108):553-61. [DOI:10.1016/j.jada.2008.01.030] [PMID]
- Wadworth M. Early life. In: Social determinants of health. Marmot M, Wilkinson RG (eds). Oxford: Oxford University Press; 1999, pp: 44-52.
- Bradley JR, Cartwright S. Social support, job stress, health, and job satisfaction among nurses in the United Kingdom. International Journal of Stress Management. 2002; 9(3):163-82. [DOI:10.1023/A:1015567731248]
- Abdollahpour S, Ramezani S, Khosravi A. Perceived social support among family in pregnant women. International Journal of Pediatrics. 2015; 3(5-1):879-88. [DOI:10.22038/ijp.2015.4703]
- Parsaierad E, Akbari AA, Mashak R. [Comparison of insomnia, sleepness, and social support in depressed and non-depressed women. New Findings in Psychology (Persian)]. 2010; 5(17):19-34. https://www.sid.ir/fa/journal/ViewPaper.aspx?id=145587
- Sarafino EP. Psychology of Health. Tehran: Roshd Publishing Co; 2008.
- Forouzandeh N, Delaram M, Deris F. [The quality of mental health status in pregnancy and its contributing factors on women visiting the health care centers of Shahrekord (Persian)]. Journal of Reproduction & Infertility. 2003; 4(2):146-55. https://www.sid.ir/fa/journal/ViewPaper.aspx?id=1108
- Green JM, Kafetsios K, Statham HE, Snowdon CM. Factor structure, validity and reliability of the Cambridge Worry Scale in a pregnant population. Journal of Health Psychology. 2003; 8:753-64. [DOI:10.1177/13591053030086008] [PMID]
- Pesonen AK, Raikkonen K, Strandberg TE, Jarvenpaa AL. Continuity of maternal stress from the pre-to the postnatal period: Associations with infants positive, negative and overall temperamental activity. Infant Behavior & Development. 2005; 28(1):36-47. [DOI:10.1016/j.infbeh.2004.09.001]
- Ross LE, Grigoriadis S, Mamisashvili L, VonderPorten EH, Roerecke M, Rehm J, et al. Selected pregnancy and delivery outcomes after exposure to antidepressant medication: A systematic review and meta-analysis. Journal of the American Medical Association Psychiatry. 2013; 70(4):436-43. [DOI:10.1001/jamapsychiatry.2013.684] [PMID]
- Kurki T, Hiilesmaa V, Raitasalo R, Mattila H, Ylikorkala O. Depression and anxiety in early pregnancy and risk for preeclampsia. Obstetrics & Gynecology. 2000; 95(4):487-90. [DOI:10.1097/00006250-200004000-00003] [PMID]
- Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Springer Publishing; 1984.
- Negahban T, Ansari A. [Does fear of childbirth predict emergency cesarean section in primiparous women (Persian)]? Hayat. 2009; 14(3-4):73-81. http://hayat.tums.ac.ir/article-1-139-en.html
- Duncombe D, Wertheim EH, Skouteris H, Paxton SJ, Kelly L. How well do women adapt to changes in their body size and shape across the course of pregnancy? Journal of Health Psychology. 2008; 13(4):503-15. [DOI:10.1177/1359105308088521] [PMID]
Article Type : Research |
Subject:
Special
Received: 2020/12/27 | Accepted: 2021/12/29 | Published: 2021/12/29
Received: 2020/12/27 | Accepted: 2021/12/29 | Published: 2021/12/29
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |