BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://hnmj.gums.ac.ir/article-1-1385-en.html
2- Assistant Professor, Department of Nursing, Trauma Nursing Research Centre, School of Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran
3- Assistant Professor, Department of Midwifery (Reproductive Health), Trauma Nursing Research Centre, Schoolof Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran
4- Assistant Professor, Department of Midwifery (Reproductive Health), Trauma Nursing Research Centre, Schoolof Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran ,
Introduction
eath anxiety is the most fundamental anxiety type among individuals [1]. It is defined as unusual and severe anxiety, i.e., associated with horror and worry when thinking about the dying process or post-death events [2]. Its’ higher prevalence among older adults is because they suffer or are prone to different physical problems, chronic conditions, impaired mobility, physical disabilities, greater dependence on others [3], significant losses (e.g., spouse, friends, & peers) [3, 4], and loneliness. Retirement and its associated loneliness can also contribute to death anxiety [4].
Most studies reported the moderate-to-high prevalence of death anxiety among older adults. A study in Turkey found that 47.5% and 52.5% of older adults suffered from mild and moderate death anxiety, respectively [5]. Another study reported that the Mean±SD score of death anxiety among American older adults was 8.3±2.6 in the possible range of 4-16 [6]. Moreover, a study in India reported that the prevalence of moderate and severe death anxiety among older adults was 60% and 40%, respectively [7]. A study on older adults in Tehran, Iran, also revealed that the Mean±SD score of death anxiety was 6.51±1.26 in the possible range of 0-15 [8].
Hospitalization, at any age, can put people in critical conditions [9, 10]. The effects of hospitalization on older adults are severer due to their greater death anxiety, lower physical energy, and lower ability to cope with unfamiliar environments [10]. Death anxiety during hospitalization and after hospital discharge is associated with different negative outcomes for the elderly. It can increase blood pressure and heart rate [11], impair mobility, undermine independence, reduce the quality of life, cause infection and death [12], and raise the odds of diagnostic errors; and consequently, prolong hospital stay, cause frequent hospitalizations, and increase hospital staff’s workload and healthcare-related costs [13].
Assessing death anxiety and determining its contributing factors during hospitalization and convalescence are essential to identify at-risk older adults, provide them with appropriate care, and facilitate their recovery and shorten their hospital stay, accordingly. Death anxiety is a multifactorial phenomenon. Its most crucial contributing factors during hospitalization include the characteristics of the hospitalization ward [14], unawareness about treatments and illness prognosis [15], limited visitation, bed arrangement in the ward [16], healthcare providers’ communication styles (especially nurses) [17], and the lack of providing necessary educations [18]. Besides, factors, such as spiritual well-being, life satisfaction, social support, educational status, age, and gender can affect death anxiety.
However, previous studies exploring the effects of these factors on death anxiety reported contradictory data. For instance, some studies reported that death anxiety had a significant positive correlation with age [7], spiritual well-being [19], and social support [19, 20]; while some other studies reported its negative correlation with spiritual well-being [8], social support [21], and age [22]. Moreover, some studies reported that it was not significantly correlated with the place of residence [5], age, educational level [21], and gender [22].
Despite the moderate-to-high prevalence of death anxiety among older adults during and after their hospitalization, studies are limited in this area. Furthermore, most studies on death anxiety were conducted in nursing homes and home settings. In addition, the results of the existing studies in this area are contradictory. Therefore, the present study aimed to assess death anxiety and its predictors among older adults during and after their hospitalization.
Materials and Methods
This cross-sectional study was conducted in 2017. The study population consisted of older patients hospitalized from 21st October to 21st December in the emergency and the medical-surgical care wards of the hospital (the only general hospital in the city) in Kashan City, Iran. The inclusion criteria for the first stage of study included consent for participation, age of ≥60 years, Iranian nationality, no diagnosed mental disorder or end-stage illness, no cognitive problem (as determined through a score >20 in the Mini-Mental State Examination scale), and the ability to establish verbal communication.
The inclusion criteria for the second stage of the study were participating in the first stage and hospitalization duration of 3 days. According to a pilot study by researchers, the average length of hospitalization was 3-5 days. The research team considered the third day when the patient stayed in the hospital and was affected by the factors influencing hospital anxiety. The inclusion criteria for the third stage of the study were participation in two prior stages and a 3-day hospitalization length.
The study exclusion criteria were voluntary withdrawal from the study, developing cognitive problems, exacerbated physical conditions, a hospital stay of >1 month, patient inaccessibility after hospital discharge, re-hospitalization during the first 7 days post-hospital discharge, being transferred to other hospitals, and death. Patients with a hospital stay of <3 days were excluded from the follow-up assessments. Sampling was performed consecutively.
The sample size was calculated based on the results of an earlier study [8]. With a precision rate of 0.14 (SD of death anxiety=1.26) and an attrition rate of 10%, a sample size of 240 participants were considered.
Five instruments were used for data collection, as follows:
1. The Mini-Mental State Examination (MMSE): This scale provides an overall estimate of the cognitive state. Its’ total score ranges from 0 to 30, and its’ higher scores represent better cognitive states [23]. Score 20 is an acceptable cutoff score for the scale [24]. The Persian psychometric validated version of this scale was used [25]. A study in Iran also reported that its Cronbach’s alpha coefficient and cutoff score were 0.73 and 21, respectively [26]. MMSE has been used in numerous studies in Iran; thus, its validity and reliability were not determined in the present study [27, 28].
2. Death Anxiety Contributing Factors Questionnaire: Three different death anxiety contributing factors questionnaires were used to assess death anxiety contributing factors at T1, T2, and T3. The first-day included items on age, gender, educational level, marital and employment status, living arrangement, financial status, the number of children, the gender of children, the number of hospitalizations, hospitalization ward, underlying illnesses, significant losses, spiritual well-being, life satisfaction, satisfaction with hospital staff’s conduct and performance, having a companion, receiving information about the underlying illnesses and their treatments from healthcare providers, the possibility of performing religious rituals during hospitalization, and satisfaction with bed arrangement.
The items of the third-day questionnaire comprised hospitalization ward, satisfaction with hospital staff’s conduct and performance, having a companion, receiving information about the underlying illnesses and their treatments from healthcare providers, the possibility of performing religious rituals during hospitalization, and satisfaction with bed arrangement. The post-discharge death anxiety contributing factor questionnaire included items on the length of hospital stay, the availability of a family caregiver, and receiving educations about medications, dietary regimen, and physical activity at the time of hospital discharge.
3. Templer Death Anxiety Scale: With fifteen items, this scale measures attitudes toward death. Its possible total score is 0–15, with higher scores representing greater death anxiety. The validity and reliability of the Persian version of this scale were confirmed in a former study [29]. Its Kuder-Richardson 20 coefficient in the present study was computed as 0.83.
4. Life Satisfaction Index-Z Scale: This is a specific scale for measuring older adults’ life satisfaction. It contains 13 items responded as “I do not know,” “Agree’, and “Disagree.” Its possible total score is 0-26, with higher scores indicating greater life satisfaction. An earlier study confirmed its construct validity through known-group comparison and confirmed its reliability with a Cronbach’s alpha coefficient of 0.79 [30]. Its split-half Spearman-Brown correlation coefficient in the present study was obtained as 0.6.
5. Spiritual Well-Being Scale: This 20-item scale consists of two main domains of religious well-being (10 items) and existential well-being (10 items). The possible total scores of the scale and each of its domains are 20-120 and 10-60, respectively. Higher scores stand for better well-being status [31, 32]. Its Cronbach’s alpha coefficient was calculated as 0.92 in our study.
Study data were collected at three time-points, namely the first hospitalization day (T1), the third hospitalization day (T2), and the seventh day after hospital discharge (T3). At T1, we assessed the hospitalized elderly for inclusion criteria, initially in terms of the cognitive state. Then, the eligible participants were requested to complete the first-day death anxiety contributing factor questionnaire, Death Anxiety Scale, Life Satisfaction Index, and the Spiritual Well-Being Scale. At T2, we re-assessed their cognitive state; then, eligible participants completed third-day death anxiety contributing factor questionnaire and the Death Anxiety Scale. Moreover, we obtained their home address, cell- and home phone numbers, and their companions’ cell phone numbers for post-discharge assessment (T3). At T3, we referred to the study participants’ homes or preferred places, re-assessed their cognitive state, and requested them to complete the post-discharge death anxiety contributing factor questionnaire and the Death Anxiety Scale. Literate participants independently responded to the study instruments, while data collection for illiterate participants was performed through face-to-face interviews by the first author.
The collected data were analyzed using SPSS. The normality of the data was evaluated via the Kolmogorov-Smirnov test. In univariable analysis, the relationship between death anxiety and two-level categorical variables was tested using the Independent Samples t-test and the Mann-Whitney U test. Furthermore, its relationship with multi-level categorical variables was tested using the one-way Analysis of Variance (ANOVA) and the Kruskal-Wallis test. The correlation between death anxiety and numerical variables (e.g., life satisfaction and spiritual well-being) was tested through Pearson’s correlation coefficient and the Spearman-Brown correlation analyses. In multivariable analysis, the stepwise multiple linear regression analysis was conducted to determine the predictors of death anxiety at T1 and T3.
Moreover, as the distribution of death anxiety scores at T2 was not normal, the predictors of death anxiety at this time-point were determined through the rank regression analysis. Repeated measures ANOVA was also used to test the differences among the three-measurement time-points respecting the mean score of death anxiety. Only those participants whose data at T1-T3 were completed were included in the repeated measures ANOVA (n=199). All statistical analyses were performed at a significance level of P<0.05
Results
Among 2290 older adults who were hospitalized during the two-month course of the study, 241 met the inclusion criteria. At T2, 13 participants were excluded due to voluntary withdrawal (n=1), transfer to critical care units (n=9), altered consciousness (n=2), and death (n=1). Moreover, at T3, 29 participants were excluded due to re-hospitalization (n=3), voluntary withdrawal (n=2), inaccessibility (n=23), and death (n=1). Therefore, the number of participants at T1, T2, and T3 was 241, 228, and 199, respectively. Table 1 presents the study subjects’ demographic characteristics.
The Mean±SD score of death anxiety among the 199 study participants whose anxiety-related data were available at T1–T3 was 6.79±3.081 at T1, 7.45±3.63 at T2, and 6.18±3.36 at T3. The repeated measures ANOVA and the Greenhouse-Geisser correction results illustrated the significant effect of time on death anxiety (F=33.08; P=0.0001). In other words, there was at least one significant difference among the three-measurement time-points respecting the mean score of death anxiety. Pairwise comparisons using the Bonferroni correction revealed that the differences between T1 and T2, T1 and T3, and T2 and T3 were statistically significant (P=0.001).
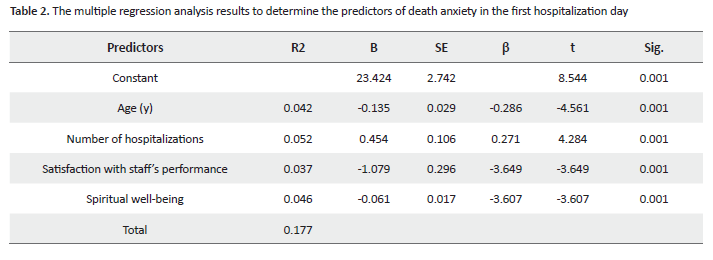
Univariable analysis results indicated that at T1, death anxiety was significantly associated with children’ gender (P=0.02), satisfaction with hospital staff’s performance (P=0.001), satisfaction with bed arrangement (P=0.04), age (P=0.001), the number of hospitalizations (P=0.01), and spiritual well-being (P=0.005). All variables which had a significant or near-significant relationship with death anxiety with P<0.2 in univariable analysis were entered into the stepwise multiple linear regression analysis. This analysis data revealed that the significant predictors of death anxiety at T1 were age, the number of hospitalizations, satisfaction with hospital staff’s performance, and spiritual well-being (F=12.50; P=0.0001) (Table 2). These 4 factors explained 17.7% of the total variance of death anxiety. The most significant predictor was the number of hospitalizations (R2=0.052). In addition, the coefficient of all factors, except for the frequency of admission was negative.
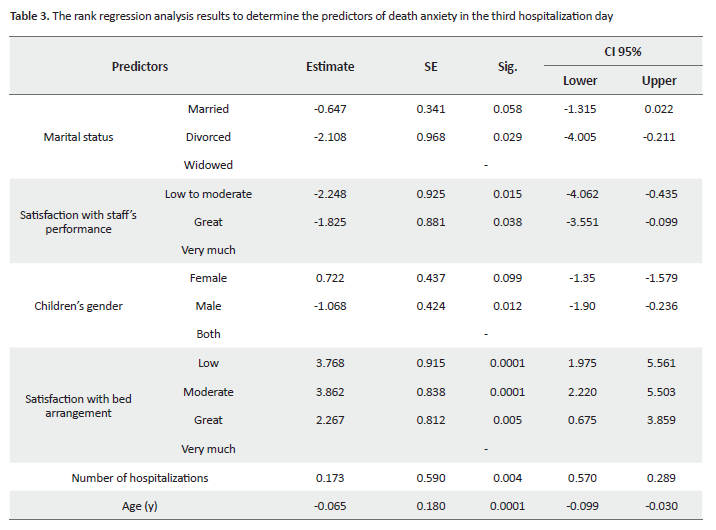
At T2, univariable analysis indicated a significant relationships between death anxiety and age (P=0.009), the number of hospitalizations (P=0.01), spiritual well-being (P=0.02), satisfaction with bed arrangement (P=0.001), receiving information about the underlying illness from healthcare providers (P=0.05), hospitalization ward (P=0.02), children’s gender (P=0.04), and having a companion (P=0.004). Multivariable analysis using the rank regression analysis on variables with P<0.2 in univariable analysis revealed that the significant predictors of death anxiety at T2 were satisfaction with bed arrangement, children’s gender, satisfaction with hospital staff’s performance, marital status, the number of hospitalizations, and age (P<0.5) (Table 3).
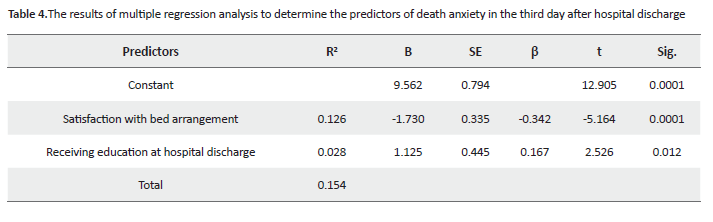
At T3, the univariable analysis revealed that death anxiety had significant relationships with the hospitalization ward (P=0.02), satisfaction with bed arrangement (P=0.001), having a companion (P=0.03), receiving education at hospital discharge (P=0.009), and age (P=0.01). Multivariable analysis through multiple linear regression on variables with P<0.05 in univariable analysis suggested satisfaction with bed arrangement and receiving education at hospital discharge as the significant predictors of death anxiety at T3 (F=17.66; P=0.0001) (Table 4). These two factors explained 15.4% of death anxiety total variance. The most significant predictor was satisfaction with bed arrangement (R2=0.126). Besides, the coefficient of satisfaction with bed arrangement was negative, and the coefficient of education during discharge was positive.
Discussion
This study assessed death anxiety and its predictors among older adults during and after hospitalization. The study findings revealed that the elderly suffered from moderate death anxiety during and one week after their hospitalization. Previous studies reported that most hospitalized patients suffered from moderate death anxiety [5-8].
Furthermore, death anxiety at the third hospitalization day was significantly greater than the first hospitalization day and the seventh day after hospital discharge. In other words, death anxiety significantly exacerbated during the hospital stay and significantly alleviated after hospital discharge. The significant exacerbation of death anxiety during hospital stay might be attributed to hospitalization-related stressors, such as separation from family, unfamiliar hospital settings, diagnostic and therapeutic interventions, healthcare providers’ poor communication with patients [33, 34], fear over survival with serious health problems, pain and discomfort, inadequate sleep, the loss of independence in performing most daily living activities, the loss of control over the environment, intrusion to personal privacy, sensory overload, reduced social contribution, the loss of respect and dignity, boredom at short visitations, and witnessing other patients’ death [35]. Consequently, death anxiety alleviation after hospital discharge might be due to the elimination of these stressors, placement in the familiar environment of family, impacting care receipt, having familiar caregivers, and improved health status.
The obtained data revealed age, the number of hospitalizations, satisfaction with hospital staff’s performance, and spiritual well-being, as the significant predictors of death anxiety at the first hospitalization day. In the present study, death anxiety alleviated with age. Numerous studies also reported the significant relationship between death anxiety and age [7, 19]. Death anxiety alleviation with age may be because older adults consider death as the termination of their problems, disabilities, pain, and impaired self-esteem; therefore, they feel less anxious over it. Our results also suggested lower death anxiety among participants with better spiritual well-being status. Previous studies also reported the significant effects of spirituality [36] and religiosity [37] on death anxiety and fear. We also found that a greater number of hospitalizations were associated with aggravated death anxiety.
An earlier study on diabetic older adults in Iran also reported the significant relationship between death anxiety and the number of hospitalizations [38]. It seems that a greater number of hospitalizations not only exhaust patients but also make them feel that they are suffering from serious conditions and reduces their hope for recovery; thus, exacerbates their death anxiety. In addition, the study participants who were more satisfied with the hospital staff’s performance had lower levels of death anxiety. Satisfaction with staff’s performance (especially nurses) is mainly affected by their conduct and communication style [39] and significantly affects patients’ sense of psychological security [40].
Study findings indicated that the significant predictors of death anxiety in the third hospitalization day included the number of hospitalizations, age, satisfaction with hospital staff’s performance, and with bed arrangement, marital status, and children’s gender. Married participants reported lower death anxiety. Similarly, an earlier study in India documented higher death anxiety among widowed men and women [20].
This finding is attributable to the fact that bachelorhood may reduce older adults’ perceived support, give them a sense of loneliness, cause them social isolation; consequently, it threatens their biopsychological health [41] and exacerbate their death anxiety. Moreover, we found that having male children was associated with lower levels of death anxiety on the third hospitalization day. This is in agreement with the findings of two earlier studies in Iran [42] and the United States [43]. This finding also highlights the effects of perceived support on death anxiety.
In eastern cultures, male children are considered as the main source of support for parents. Therefore, older adults with male children may feel greater support, have a greater feeling of security, and experience less death anxiety. Another study finding was that the study participants’ satisfaction with bed arrangement was associated with decreased death anxiety on the third hospitalization day. Older adults may value the arrangement of ward beds according to the patients’ language, culture, age, and physical health status; thus, they feel less death anxiety when placed close to the patients of their language, culture, and age group.
We also found that on the seventh day after hospital discharge, the significant predictors of death anxiety were satisfaction with bed arrangement and receiving education at hospital discharge. A study in Iran [44] also reported the effectiveness of preoperative education in significantly alleviating anxiety. Besides, another study reported that lack of education can cause anxiety among patients.
Unawareness about illness, its prognosis, and treatments, as well as hospital settings and medical equipment, were among the leading causes of anxiety and stress among hospitalized patients [45]. Education helps correct misconceptions about health, illnesses, and treatment; accordingly, it alleviates anxiety. Patients undergoing training and counseling at discharge feel ready for discharge. This readiness can be effective in reducing post-discharge anxiety.
In patients’ arrangement in the ward, placing the elderly patient alongside these patients; dead, illness, despair about treatment, and having a negative attitude toward treatment staff could increase the anxiety of death after discharge.
Among the strengths of the study was death anxiety assessment at several measurement time-points and data analysis via the multiple regression analysis. On the other hand, the main study limitations were consecutive sampling from a single hospital and excluding some participants due to their inaccessibility after hospital discharge. Thus, multi-center studies with larger sample sizes are recommended to evaluate and compare death anxiety among hospitalized elderly, nursing home residents, and community-dwelling older adults.
Older adults experience moderate anxiety during and after their hospitalization. Their death anxiety significantly exacerbates during their hospital stay and significantly alleviates after hospital discharge. The significant predictors of death anxiety during hospital stay included the number of hospitalizations, satisfaction with hospital staff’s performance, spiritual well-being, marital status, children’s gender, satisfaction with bed arrangement, and age. Furthermore, its significant predictors after hospital discharge were satisfaction with bed arrangement and receiving education at hospital discharge. Therefore, developing and employing culturally-appropriate strategies to enhance hospitalized older adults’ satisfaction with hospital staff’s performance and bed arrangement and providing them with necessary educations at hospital discharge are recommended to alleviate their death anxiety.
Ethical Considerations
Compliance with ethical guidelines
Approvals for this study were obtained from the Ethics Committee and the Institutional Review Board of Kashan University of Medical Sciences, Kashan, Iran (Codes: Kashan.1396.10 & 1396.07.25.9662). Permissions were also obtained from the authorities of this university and provided to the authorities of the study setting. The study purpose was clearly explained to the study participants and the authorities of the study setting. All study participants were ensured about confidential data handling, anonymous data reporting, and voluntary participation in the study.
Funding
This study was supported by the Research and Technology Administration of Kashan University of Medical Sciences, Kashan, Iran.
Authors contributions
Designation of the study: Zahra Tagharrobi, Khadijeh Sharifi, and Zahra Sooki; Data collection: Zahra Zahedi Bidgoli; Data analysis: Zahra Zahedi Bidgoli. Writing of the manuscript and approving the final version of the manuscript: All the authors.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgements
We would like to thank all participating older adults as well as the Research and Technology Administration of Kashan University of Medical Sciences for their support.
References
- Fritsche I, Jonas E, Kayser DN, Koranyi N. Existential threat and compliance with pro-environmental norms. Journal of Environmental Psychology. 2010; 30(1):67-79. [DOI:10.1016/j.jenvp.2009.08.007]
- Rahmani M. The relationship between life expectancy and resilience with death anxiety in dengue patients, unpublished thesis. Tonekabon, Department of Psychology. Tonekabon: Islamic Azad University; 2012.
- Nayak S, Mohapatra MK, Panda B. Prevalence of and factors contributing to anxiety, depression and cognitive disorders among urban elderly in Odisha: A study through the health systems’ Lens. Archives of Gerontology and Geriatrics. 2019; 80:38-45. [DOI:10.1016/j.archger.2018.09.008] [PMID]
- Aghajani M, Valiee S, Tol A. Death anxiety amongst nurses in critical care and general wards. Iran Journal of Nursing (IJN) 2011; 23(67):59-68.
- Sridevi G, Swathi P. Death anxiety and death depression among institutionalized and non-Institutionalized elders. International Journal of Scientific and Research Publications. 2014; 4(10):1-8.
- Krausa N, Bastida E. Contact with the dead, religion, and death anxiety among older Mexican Americans. Death Studies. 2012; 36(10):932-48. [DOI:10.1080/07481187.2011.604468] [PMID] [PMCID]
- John M, Binoy S, Reddy JV, Passyavula SK, Reddy VP. A study to assess the level of death anxiety among elderly people at selected area at Bhopal. International Journal of Medical and Health Research. 2016; 2(5):23-4.
- Moetamedi A, Pajouhinia S, Fatemi Ardestani M. [The impact of spiritual wellbeing and resiliency in predicting death anxiety among elderly people in Tehran (Persian)]. Shefaye Khatam. 2015; 3(2):19-26. [DOI:10.18869/acadpub.shefa.3.2.19]
- Rangraz JF, Akbari H Rasoli S. Older people home care through electronic health records: Functions, data elements and security needs. Contemp Nurse. 2016; 52(2-3):352-65. [DOI:10.1080/10376178.2016.1213649] [PMID]
- Rejeh N, Heravi-Karimooi M, Foroughan M. [The needs of hospitalized elderly patients: A qualitative study (Persian)]. Salmand: Iranian Journal of Ageing. 2010; 5(1):42-52.
- Moradyan T, Ebadi A, Saeid Y, Asiabi M. [Hospital anxiety and depression in patients with coronary artery disease (Persian)]. Journal of Nursing Education. 2013: 1(2):54-61.
- Fernandez-Sierra MA, Rueda-Domingo MT, Rodriguez-Del-Aguila MM, Perez-Lozano MJ, Force L, Fernandez-Villa T, et al. Adaptation of antibiotic treatment to clinical practice guidelines in patients aged⩾65 years hospitalised due to community-acquired pneumonia. Epidemiology Infection. 2018; 146(14):1870-7. [DOI:10.1017/S0950268818002121] [PMID]
- Shojaei A, Akbari-Kamrani AA, Fadaye-Vatan R, Azimian M, Ghafari Sh, Jamali MR. [Medical costs and illnesses in the elderly covered by the Health Insurance Agency, Tehran province (2008-2009) (Persian)]. Salmand. 2012; 6(22):65-74.
- Jariani M, Saki M, Momeni M, Ebrahimzadeh F, Seydian A. [The effect of progressive muscle relaxation techniques on anxiety in patients with myocardial infarction (Persian)]. Yafte. 2011; 13(3):22-30.
- Zamanzadeh V, Valizadeh L, Mohajjel Aghdam A, Reza Gholifam A. [Actual patient education: Nurse’s perception of tabriz teaching hospitals (Persian)]. Nursing and Midwifery Journal. 2010; 5(19):39-46.
- Hunter JD, Goddard C, Rothwell M, Ketharaju S, Cooper H. A survey of intensive care unit visiting policies in the United Kingdom. Anaesthesia. 2010; 65(11):1101-5. [DOI:10.1111/j.1365-2044.2010.06506.x] [PMID]
- Haugan G, Innstrand ST, Moksnes UK. The effect of nurse-patient interaction on anxiety and depression in cognitively intact nursing home patients. Journal of Clinical Nursing. 2013; 22(15-16):2192-205. [DOI:10.1111/jocn.12072] [PMID]
- Farahaninia M, Abbasi M, Givari A, Haghani H. [Nursing students’ spiritual well-being and their perspectives towards spirituality and spiritual care perspectives (Persian)]. Iran Journal of Nursing. 2006; 18(44):7-14.
- Harrawood LK, White LJ, Benshoff JJ. Death anxiety in a national sample of United States funeral directors and its relationship with death exposure, age, and sex. Omega Journal of Death Dying. 2008-2009; 58(2):129-46. [DOI:10.2190/OM.58.2.c] [PMID]
- Ghufran M, Ansari S. Impact of widowhood on religiosity and death anxiety among senior citizens. Journal of the Indian Academy of Applied Psychology. 2008; 34:175-80.
- Nouhi E, Karimi T, Iranmanesh S. [Comparing fear of death of the elderly settled in elderly’s home and inhabited in city houses of Isfahan (Persian)]. Iranian Journal of Ageing. 2014; 8(4):24-31.
- Azaiza F, Ron P, Shoham M, Gigini I. Death and dying anxiety among elderly Arab Muslims in Israel. Death Studies. 2010; 34(4):351-64. [DOI:10.1080/07481181003613941] [PMID]
- Lin LC, Watson R, Lee YC, Chou YC, Wu SC. Edinburgh Feeding Evaluation in Dementia (EdFED) scale: Cross‐cultural validation of the Chinese version. Journal of Advanced Nursing. 2008; 62(1):116-23. [DOI:10.1111/j.1365-2648.2008.04596.x] [PMID]
- Wu Ch, Yao G. Psychometric analysis of the short-form UCLA Loneliness Scale (ULS-8) in Taiwanese undergraduate students. Personality and Individual Differences. 2008; 44(8):1762-71. [DOI:10.1016/j.paid.2008.02.003]
- Seyedian M, Falah M, Nourouzian M, Nejat S, Delavar A, Ghasemzadeh HA. [Validity of the Farsi version of mini-mental state examination (Persian)]. Journal Of Medical Council of I.R.I. 2008; 25(4):408-14.
- Ghazanfari F, Hashemi Sh, Sepahvand R. [The survey for relation between cognitive status and life quality in older people at army retired community in Khorram Abad 2011 (Persian)]. Journal of Nurse and Physician within War. 2013; (21-22):11-16.
- Rezaie-Nasab T, Salehi I, Kafi M, Rezaie S. The validity, diagnostic value and replicability of bender visual-motor gestalt test in traumatic brain injury patients. Hormozgan Medical Journal. 2014; 18(4):297-308.
- Taheri-Tanjani P, Azadbakht M. [Psychometric properties of the Persian version of the activities of daily living scale and instrumental activities of daily living scale in elderly (Persian)]. Journal of Mazandaran University of Medical Sciences. 2016; 25(132):103-12.
- Bitarafan L, Kazemi M, Yousefi-Afrashte M. [Relationship between styles of attachment to god and death anxiety resilience in the elderly (Persian)]. Salmand Iranian Journal of Ageing. 2018; 12(4):446-57. [DOI:10.21859/sija.12.4.446]
- Tagharrobi Z, Sharifi K, Tagharrobi L, Sooky Z. Psychometric evaluation of the satisfaction index-z in Iranian elderly. European Psychiatry. 2008; 23(2):S399-S400. [DOI:10.1016/j.eurpsy.2008.01.1382]
- Bamdad M, Fallahi-Khoshknab MR, Dalvandi A, Khodayi-Ardakani MR. [Impact of spiritual care on spiritual health of hospitalized amphetamin dependents (Persian)]. Iranian Journal of Psychiatric Nursing. 2013; 1(3):10-8.
- Bastani F, Pourmohammadi A, Haghani H. [Relationship between perceived stress with spiritual health among older adults with diabetes registered to the association of diabetes prevention and control in Babol, 2013 (Persian)]. Journal of Hayat. 2014; 20(3):6-18.
- Musavi Z, Alavi M, Alimohammadi N, Hosseini H. Development and initial psychometric evaluation of the hospitalization-related stressors questionnaire for elderly patients. Iranian Journal of Nursing and Midwifery Research. 2016; 21(5):516-20. [DOI:10.4103/1735-9066.193416] [PMID] [PMCID]
- Nasirizade M, Hosseini M, Biabani F, Geraminejad N. [Assessment of nurses’ performance regarding patient education from patients’ standpoint (Persian)]. Scientific Journal of Education Strategies in Medical Science. 2018; 11(4):123-8.
- Ahmadi, MH. [Pathology of stress and control methods: How to be calm (Persian)]. 1st edition. Nazar Abad: Siyadat; 2014.
- Hedayati E, Hazrati M, Momen-Nasab M, Shokoohi H, Afkari F. [The relationship between spiritual well-being and anxiety of aged people admitted in coronary care units (Persian)]. Iranian Journal of Ageing, 2016; 11(3):432-9. [DOI:10.21859/sija-1103432]
- Zanjari N, Sharifian Sani M, Hosseini-Chavoshi M, Rafiey H, Mohammadi-Shahboulaghi F. Perceptions of successful Ageing Among Iranian Elders: Insights from a qualitative study. The International Journal of Aging and Human Development. 2016; 83(4):381-401. [DOI:10.1177/0091415016657559] [PMID]
- Azadi A, Taghinezhad H, Bastami M, Bastami AR, Pashaei-Sabet F. [Depression among elderly diabetic patients referred to Shahid Mostafa Khomeini in Ilam Shohada Ashayer Hospitals in Khoramabad 2015 (Persian)]. Iraqnian Journal of Nursing Research. 2016; 11(3):1-9.
- Jacelon CS. Managing personal integrity: The process of hospitalization for elders. Journal of Advanced Nursing. 2004; 46(5):549-57. [DOI:10.1111/j.1365-2648.2004.03029.x] [PMID]
- Newell S, Jordan Z. The patient experience of patient-centered communication with nurses in the hospital setting: A qualitative systematic review protocol. JBI Database of Systematic Reviews Implementation Reports. 2015; 13(1):76-87. [DOI:10.11124/jbisrir-2015-1072] [PMID]
- Nabavi Sh, Alipour F, Hejazi A, Rabbani E, Rashedi V. [Relationship between social support and mental health in older adults (Persian)]. Medical Journal of Mashhad University of Medical Sciences. 2014; 57(7):841-6.
- Masoudzadeh A, Setareh J, Mohammadpour RA, Modanloo-Kordi M. [A survey of death anxiety among personnel of a hospital in Sari (Persian)]. Journal of Mazandaran University of Medical Sciences. 2008; 18(67):84-90.
- Pierce JD, Cohen A, Chamber JA, Meade RM. Gender differences in death anxiety and religious orientation among US high school and college students. Mental Health, Religion Culture. 2007; 10(2):143-50. [DOI:10.1080/13694670500440650]
- Zare-Marzouni H, Karimi M, Narimi Zh, Ghasemi A, Janaki M. [Effects of education on reduction of stress and anxiety of orthopedic surgery (Persian)]. Navid. 2016; 16(62):62-8.
- Chien WT, Leung SF. A controlled trial of a needs‐based, nurse‐led psychoeducation programme for Chinese patients with first‐onset mental disorders: 6 month follow up. International Journal of Nursing Practice. 2013; 19( Suppl 1):3-13. [DOI:10.1111/ijn.12015] [PMID]
Received: 2020/03/30 | Accepted: 2020/03/30 | Published: 2020/03/30
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |