BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://hnmj.gums.ac.ir/article-1-1384-en.html
2- Assistant Professor, Department of Nursing, School of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran ,
3- MsN, RN, Nikookari Hospital, Tabriz University of Medical Sciences, Tabriz, Iran
Introduction
laucoma or ocular hypertension refers to a group of diseases that damage the optic nerves. This damage is caused by the increased blood pressure within the eye, i.e., resulted from aqueous humor hyperemia. This damage finally leads to reduced vision or blindness. In glaucoma cases, the optic nerve progressive damage initially manifests with reduced peripheral vision. Without timely diagnosis and treatment, this damage can lead to a reduction in the central vision and blindness [1].
The prevalence of glaucoma in people aged >50 years is estimated to be 1.5% to 2% globally. The prevalence of this disease increases with age, and among people aged >80 years, its’ prevalence is between 2% to 10% [2]. The prevalence of this disease among individuals aged 40-49 and >80 years in Iran is reported to be 0.5% and 5%, respectively [3].
Glaucoma is recognized as the “silent thief” because the majority of patients remain unaware of their disease until they observe changes and a decline in vision. Glaucoma is a chronic disease that requires lifetime care. Uncontrolled glaucoma may lead to blindness [4]. Long-term treatment of glaucoma cannot compensate for the losses and cannot improve vision. However, treatment can prevent the advancement of the damage and aggravate the patient’s condition [5]. The objective of glaucoma treatments is to maintain visual performance. Ophthalmology indicators, such as visual acuity and visual field assessment, are used to evaluate treatment outcomes [6]. These indicators reflect the treatment success rate; however, they are considered to be incomplete, as they fail to reflect the patients’ awareness of the disease. Different studies in several countries investigated the relationship between quality of life and visual performance. The majority of these studies have approved the existence of such a relationship [7].
The interest in measuring life quality, as a health consequence, has increased worldwide with the improved advancements in different life dimensions [8]. A research conducted in 2008-2009 in the Nour Hospital of Tehran revealed that the quality of life score obtained by healthy individuals was significantly higher than that of the patients with chronic ocular diseases in all vision fields [9]. Compared to other studies, the quality of life of the patients in this research was lower than in others [8, 10].
A study revealed that self-management is an active, practical process led by patients with glaucoma. This active process includes behavioral monitoring activities and skills meant to improve health and well-being; prevent disease complications, consult with healthcare providers on cooperative decisions; confront negative emotional states, and contribute to the continuation of constructive social roles in interpersonal relations and job positions to attain self-management goals. Self-management positively contributes to the quality of life of many patients with chronic diseases [10].
Another study examined the self-management of patients with glaucoma and indicated that receiving self-management skills decreased anxiety symptoms and increased life quality in patients. Self-management is a highly effective measure, i.e., especially useful for old patients suffering from ocular disorders and depression. In other words, self-management has a long-term positive effect on the quality of life [10, 11]. Self-management, which is widely accepted as a new superior model of management and treatment of chronic diseases in the world, reflects the revolutionary shift from passive surrender to active participation in managing chronic diseases. Some relevant studies that have focused on chronic diseases revealed that self-management guarantees the quality of life [11]. As the patients’ awareness of their problems increases, they more actively participate in the management of their diseases [4].
Few studies have been conducted in Iran to determine the relationship between self-management and the quality of life and visual performance in patients with glaucoma. Glaucoma greatly influences the quality of life of patients. Moreover, different scores have been reported by various researchers for the quality of life of patients with glaucoma. Thus, the relationship between self-management behaviors and the quality of life and visual performance of patients remains unclear. The present study results may help to improve self-management in patients with glaucoma. This research aimed to determine the relationship between self-management and the quality of life and visual performance among patients with glaucoma referring to the eye Hospital of Tabriz City, Iran.
Materials and Methods
A cross-sectional, comparative study was conducted in the Eye Hospital affiliated to the Tabriz University of Medical Sciences from May to August 2016. The study participants were selected through simple random sampling method. Potential participants who met the inclusion criteria were invited to participate in the study. Written and verbal information about the study was provided prior to the commencement study. The inclusion criteria included being aged >18 years, patients suffering at least 6 months from glaucoma, and approving glaucoma diagnosis by a physician. There were no participants excluded based on gender or ethnicity. According to the variables of a previous study (quality of life SD= 1.8; Z=1.96; D= 0.3), the sample size was calculated [9], and 120 patients meeting the inclusion criteria were included in the study.
The required data were collected using a 4-section questionnaire. Part one comprised of questions on the participants’ demographic characteristics; part two was the National Eye Institute-Visual Functioning Questionnaire (NEI-VFQ); part 3 was the Glaucoma Quality of Life (GQOL-15), and part 4 was the Patient Activation Measure (PAM) to assess the self-management and self-confidence skills of patients.
The NEI-VFQ comprised of 39 questions classified into 12 subscales, including general health, general vision, near activity, distance activity, vision-specific social functioning, driving, vision-specific role difficulties, peripheral vision, color vision, vision-specific mental health, ocular pain, and vision-specific dependency. The scale’s total score ranges from 0 (the worst function) to 100 (the best function) [12].
GQOL-15 includes 6 items relating to actions demanding functional peripheral vision; 6 relating to dark adaptation and glare; two relating to central and
near vision, and one relating to outdoor mobility. Each question’s answer is scored from 1 (without problem) to 5 (severe problem). Total minimum and maximum scores of this scale are 15 and 75, respectively [13].
PAM is comprised of 22 items divided into 4 subscales, including believes active role is important; confidence and knowledge to taking action; taking action, and staying the course under stress. The questions were answered using a 5-item Likert-type scale ranging from [1] completely disagree to [5] completely agree. The scale’s total score ranges from 0 to 100; it is divided into 4 levels, including 0-25 (level I), 25-50 (level II), 50-75 (level III), and 75-100 (level IV) [14].
The inventory’s content validity was established by the comments of the panel of 10 experts in the field of nursing and ophthalmology. After filling 20 questionnaires by patients, Cronbach’s alpha coefficient was used to determine the internal consistency of the questionnaire, scoring 0.71 for the whole questionnaire, and 0.92 for the GQOL, 0.93 for the NEI-VFQ, and 0.52 for the PAM subscale.
Ethical approval was obtained from the Ethics Committee of Tabriz University of Medical Sciences . However, the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist was used to determine the items that should be included in the report of this cross-sectional study.
The obtained data were analyzed in SPSS V. 16. The study participants’ demographic information was analyzed using frequency, percentage, Mean±SD. Student Samples t-test and Pearson’s correlation coefficient were conducted to compare mean scores and determine the study variables’ relations. P<0.05 was considered as statistically significant.
Results
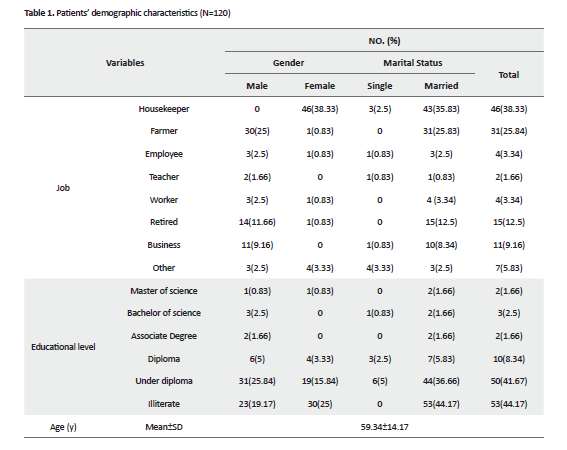
In total, 55% of the study patients were male, 91.3% were married, 17.5% reported a family history of the disease, and 82.5% reported no family history of glaucoma. The Mean±SD age of the study participants was 59.34±14.17 years. Patients’ demographic characteristics are presented in Table 1.
The total Mean±SD score of the quality of life among glaucoma patients was 33.88±13.73; and the highest score of the quality of life belonged to peripheral vision and adaption to darkness (13.85±6.29), while the minimum score belonged to mobility in open spaces (2.19±1.19). The total Mean±SD score of self-management obtained by patients with glaucoma was 65.06±12.69; and the highest score of self-management belonged to the patients with the highest confidence and knowledge to taking action (30.75±4.43), while the lowest Mean±SD belonged to the active role of beliefs (7.2±1.28). Furthermore, 60.8% of the study patients were in level 4, 15.8% were in level 3, 12.5% in level 2, and 10.9% were in level 1 of self-management. However, the total Mean±SD score of visual performance was 81.36±14.01; and the highest mean score±SD of visual performance belonged to color vision (84.16±25.71), while the lowest Mean±SD score belonged to ocular pain (59.26±1.22) (Table 2).
Moreover, there was a significant relationship between self-management and the quality of life and visual performance in these patients (r= 0.420, r= 0.240, P=0.001, respectively). Additionally, there was no significant gender difference in terms of self-management, the quality of life, and visual performance (P=0.066, P=0.071 & P=0.160, respectively) (Table 3).
Discussion:
The current study examined the relationship between self-management and the quality of life and visual performance in patients with glaucoma referring to the eye Hospital of Tabriz City, Iran. The obtained results revealed a significant and linear relationship between self-management and the quality of life and visual performance in the study subjects. In addition, the Mean±SD score of the quality of life among glaucoma patients was 33.88±13.73 and the majority of patients obtained the highest mean values for adapting to darkness and peripheral vision.
The lowest mean values also belonged to movement in open spaces and central vision. In the study by Onakoya et al., in which similar tools were used to determine the quality of life of patients with glaucoma, the relative value was 24.07±12.2, and the patients’ major problem was adapting to darkness and glare. The quality of life of such patients was reported to be lower than that of healthy individuals [15]. According to Goldberg et al., the quality of life of patients with glaucoma was significantly lower than that of healthy individuals. They also reported a significant relationship between life quality and severity of disease in this group [16].
A study was conducted from 2008 to 2009 in Tehran to examine the relationship between life quality and vision in patients with chronic ocular diseases. The investigators reported that the highest score of life quality belonged to patients with a 20/70 vision or lower. In this study, the quality of life scores of participants was lower than those of participants in other countries [9]. The largest average values of self-management in this study belonged to patients with the confidence and awareness of glaucoma management. Thus, with an increase in the awareness of patients, their quality of life improves.
The findings of the present research indicated that patients’ awareness of the nature of glaucoma significantly impacts the management of glaucoma and life quality of patients. Therefore, these findings comply with those of other relevant studies. A study explored the knowledge, attitude, and self-care practices of patients with glaucoma in South Africa. The relevant results revealed that the patient’s awareness of the nature of the disease is highly important. Moreover, appropriate knowledge of glaucoma was significantly associated with desirable self-care practices of glaucoma [17].
Another study assessed the patients’ awareness and knowledge of glaucoma in a referral teaching hospital in Ghana. It was concluded that there were statistically significant differences between those who had higher education and awareness of glaucoma. However, only 27% of them reported accurate knowledge of glaucoma [18]. According to Aghedo et al., elderly patients have insufficient knowledge of glaucoma and have poor self-care glaucoma practices. It is important to involve the family members of these patients in the education and counseling of glaucoma to facilitate improved disease management [17].
Based on the present study findings, the highest mean value belonged to color vision, while the lowest belonged to ocular pain and mental health. Zhou et al. examined the quality of life of patients with glaucoma. The researchers stated that anxiety and depression were prevalent among glaucoma patients and consequently led to a decline in their performance and life quality [19]. Another study explored the life quality and visual performance of patients with glaucoma in Greece. The life quality and visual performance scores obtained by the patients were different from those of the present study [20]. In the present research, the most significant problems of patients with glaucoma were mental health (anxiety and depression) and ocular pain. Besides, the visual performance of patients directly influenced their quality of life.
The current study results revealed a linearly significant relationship between self-management and life quality and visual performance in the studied patients. Wu et al. performed a multiple linear regression analysis studies. They revealed that self-management behavior, positive family records of glaucoma, and binocular visual performance were the predictors of the life quality associated with vision in these patients. Their results also indicated that the quality of life associated with vision in patients with glaucoma in China was at the average level. However, self-management behavior is an essential predictor in this regard [11]. The achieved results indicated that the level of self-management was high among patients with glaucoma.
Furthermore, the highest mean values belonged to the confidence and awareness of patients. Most patients had a moderate quality of life, and the highest mean score belonged to peripheral vision, sensitivity to light, and adaptation to darkness. Moreover, the overall visual performance of patients with glaucoma was acceptable and color vision having the highest average score. The relationship between self-management and the quality of life and visual performance of patients with glaucoma was also found to be statistically significant.
The hospital used for this study was the educational and general hospital serving the lower and middle-class population to limit the generalizability of the obtained data.
There was a significant linear relationship between self-management and the quality of life and visual performance of the studied patients; thus, considering self-management strategies in patient education plans for nursing curriculums and hospitals’ education programs are suggested.
Ethical Considerations
Compliance with ethical guidelines
The present research was approved by the Tabriz University of Medical Sciences (Code: 5/4/2173).
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors contributions
Contributions to conception and design, acquisition of data:Hadi Hassankhani, Fatemeh Heidarnejad; Analysis and interpretation of data: Hadi Hassankhani, Fatemeh Heidarnejad, and Hamidreza Haririan; Drafting the article or revising it critically:Hamidreza Haririan, Fatemeh Heidarnejad.
Conflict of interest
The authors declared no conflicts of interest.
References
- Schacknow PN, Samples JR. The glaucoma book: A practical, evidence-based approach to patient care. New York: Springer Science & Business Media; 2010 . [DOI:10.1007/978-0-387-76700-0]
- Hagman J. Resource utilization in the treatment of open angle glaucoma in Finland: An 11-year retrospective analysis. Oulu: University of Oulu; 2012.
- Mohammadi SF, Saeedi-Anari G, Alinia C, Ashrafi E, Daneshvar R, Sommer A. Is screening for glaucoma necessary? A policy guide and analysis. Journal of Ophthalmic & Vision Research. 2014; 9(1):3-6.
- Abdull MM, Chandler C, Gilbert C. Glaucoma. The silent thief of sight: Patients’ perspectives and health seeking behavior in Bauchi, Northern Nigeria. BMC Ophthalmology. 2016; 16(1):1-9. [DOI:10.1186/s12886-016-0220-6] [PMID] [PMCID]
- Sawada H. Fukuchi T, Abe H. Evaluation of the relationship between quality of vision and visual function in Japanese glaucoma patients. Graefe's Archive for Clinical and Experimental Ophthalmology. 2011; 249(11):1721-7. [DOI:10.1007/s00417-011-1779-5] [PMID]
- Dhawan M, Hans T, Sandhu PS, Midha N. Evaluation of vision-related quality of life in patients with glaucoma: A hospital-based study. Journal of Current Gaucoma Practice. 2019; 13(1):9-15. [DOI:10.5005/jp-journals-10078-1242] [PMID] [PMCID]
- Sawada H, Yoshino T, Fukuchi T, Abe H. Assessment of the vision-specific quality of life using clustered visual field in glaucoma patients. Journal of Glaucoma. 2014; 23(2):81-7. [DOI:10.1097/IJG.0b013e318265bbdc] [PMID]
- Na KS, Han K, Park YG, Na C, Joo CK. Depression, stress, quality of life, and dry eye disease in Korean women: A population-based study. Cornea. 2015; 34(7):733-8. [DOI:10.1097/ICO.0000000000000464] [PMID]
- Asgari S, Nedjat S, Hashemi H, Shahnazi A, Fotouhi A. Quality of life in the group of patients with chronic eye disease. Iranian Journal of Epidemiology. 2012; 7(4):43-48.
- Quaranta L, Riva I, Gerardi C, Oddone F, Floriano I, Konstas AG. Quality of life in glaucoma: A review of the literature. Advances in Therapy. 2016; 33(6):959-81. [DOI:10.1007/s12325-016-0333-6] [PMID] [PMCID]
- Wu P, Xi S, Xia H, Lu H, Guo W. Survey on vision-related quality of life and self-management among patients with glaucoma. Journal of Glaucoma. 2014; 23(2):75-80. [DOI:10.1097/IJG.0b013e318265bbf3] [PMID]
- Asgari S, Hashemi H, Nedjat S, Shahnazi A, Fotouhi A. Persian version of the 25-item National Eye Institute visual functioning questionnaire (NEI-VFQ 39): a validation study. Iranian Journal of Ophthalmology. 2011; 23(3):5-14.
- Loon SC, Jin J, Jin Goh M. The relationship between quality of life and adherence to medication in glaucoma patients in Singapore. Journal of Glaucoma. 2015; 24(5):e36-42. [DOI:10.1097/IJG.0000000000000007] [PMID]
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research. 2004; 39(4 Pt 1):1005-26. [DOI:10.1111/j.1475-6773.2004.00269.x] [PMID] [PMCID]
- Onakoya AO, Mbadugha CA, Aribaba OT, OO. Quality of life of primary open angle glaucoma patients in Lagos, Nigeria: Clinical and socio-demographic correlates. Journal of Glaucoma, 2012; 21(5):287-95. [DOI:10.1097/IJG.0b013e31820d7cfd] [PMID]
- Goldberg I, Clement CI, Chiang TH, Walt JG, Lee LJ, Graham S, et al. Assessing quality of life in patients with glaucoma using the glaucoma quality of life-15 (GQL-15) questionnaire. Journal of Glaucoma, 2010; 18(1):6-12. [DOI:10.1097/IJG.0b013e3181752c83] [PMID]
- Aghedo AV, Tlou B, Mahomed S. Knowledge, attitudes and self-care practices of patients with glaucoma in uThungulu in KwaZulu-Natal. African Vision and Eye Health. 2018 ;77(1):1-6. [DOI:10.4102/aveh.v77i1.442]
- Nkum G, Lartey S, Frimpong C, Micah F, Nkum B. Awareness and knowledge of glaucoma among adult patients at the eye clinic of a teaching hospital. Ghana Medical Journal. 2015; 49(3):195-9. [DOI:10.4314/gmj.v49i3.11] [PMID] [PMCID]
- Zhou C, Qian S, Wu P, Qiu C. Anxiety and depression in Chinese patients with glaucoma: socio-demographic, clinical, and self-reported correlates. Journal of Psychosomatic Research. 2013; 75(1):75-82. [DOI:10.1016/j.jpsychores.2013.03.005] [PMID]
- Labiris G, Katsanos A, Fanariotis M, Zacharaki F, Chatzoulis D, Kozobolis VP. Vision-specific quality of life in Greek glaucoma patients. Journal of Glaucoma. 2010; 19(1):39-43. [DOI:10.1097/IJG.0b013e31819d5cf7] [PMID]
Received: 2020/03/30 | Accepted: 2020/03/30 | Published: 2020/03/30
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |