Tue, Jul 9, 2024
Volume 29, Issue 4 (9-2019)
JHNM 2019, 29(4): 228-235 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Papi S, Karimi Z, Zilaee M, Shahry P. Malnutrition and Its Relation to General Health and Multimorbidity in the Older People. JHNM 2019; 29 (4) :228-235
URL: http://hnmj.gums.ac.ir/article-1-1022-en.html
URL: http://hnmj.gums.ac.ir/article-1-1022-en.html
1- PhD Student of Gerontology, Department of Health Education and Promotion, School of Health and Nutrition, Tabriz University of Medical Sciences, Tabriz, Iran.
2- Instructor, Department of Health Education and Promotion, School of Health, Qom University of Medical Science, Qom, Iran.
3- Assistant Professor, Department of Nutritional Science, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
4- Instructor, Social Determinants of Health Research Center, School of Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. ,shahry_2001@yahoo.com
2- Instructor, Department of Health Education and Promotion, School of Health, Qom University of Medical Science, Qom, Iran.
3- Assistant Professor, Department of Nutritional Science, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
4- Instructor, Social Determinants of Health Research Center, School of Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. ,
Full-Text [PDF 539 kb]
(2579 Downloads)
| Abstract (HTML) (4848 Views)
Full-Text: (1349 Views)
Introduction
alnutrition is usually defined as a faulty or bad nutritional status, which has adverse effects on the health and the quality of life of the older people [1]. In addition, it imposes a high cost on health care systems [2]. Malnutrition is an essential component of geriatric care [1]. Older people are vulnerable to malnutrition, and it is one of the common problems in this age group [3, 4]. Its prevalence in healthy older people is (5-10%), in older patients (30-60%), and in older people living in nursing homes (2-74%) depending on the assessment method [4]. In Iran, the prevalence of malnutrition has been reported (9.2%) among older people living independently and (26.1%) among those living in nursing homes [5]. Recent studies have identified several predisposing factors for malnutrition in older people, including demographic characteristics, economic conditions, diet, appetite, disease, social factors, and healthy behaviors [1, 6]. Inadequate nutritional status predisposes older people to develop diseases such as osteoporosis, diabetes, cardiovascular disease, and high blood pressure and incur higher health costs [7].
On the other hand, these people usually suffer from one or more diseases at the same time, and recent studies have reported the prevalence of multimorbidity in the elderly as (56-67%) [8-10]. Malnutrition is crucial both for the health system and for the patient as it reduces the quality of life, causes longer stay in hospital and higher costs and mortality rate [11, 12]. The presence of various diseases in older people and their poor general health status are effective and predictors of malnutrition [13-15]. According to studies conducted in Iran, the general health status of older people is moderate or undesirable. One study reported that (61.7%) of them had a poor health status [16]. Despite the growth of the elderly population in Iran and change in the population pyramid, less attention has been paid to the general health status of older people as a vulnerable group [17].
Regarding what was discussed, the study of nutritional status in older people living in nursing homes in order to identify general problems and factors associated with their malnutrition can enrich our knowledge about the aging and its threatening factors. On the other hand, providing health and identifying the needs of the elderly requires a comprehensive and accurate understanding of their health status. Furthermore, considering the aging of the population in the future, the prevalence of malnutrition among older people, and particularly in nursing homes, it is crucial to pay more attention to this issue [5]. By studying the relationship between nutritional status, general health, and multimorbidity, it is possible to design interventions to influence factors associated with malnutrition and thus reduce its prevalence. A few studies have evaluated the prevalence of malnutrition concerning general health and multimorbidity among older people in Iran. In this regard, this study aimed to assess this issue among older people living in nursing homes of Ahvaz City, Iran.
Materials and Methods
This is an analytical cross-sectional study. Study population consisted of all 250 older people living in 4 nursing homes in Ahvaz City, who were selected using the census method and met the inclusion criteria as follows: able to speak; informed consent to participate in the study; age >60 years; no Alzheimer disease, memory impairment, or dementia (according to the medical records); and not participating in other studies. The exclusion criterion was their unwillingness to continue the study. Based on these criteria, 184 older people were entered into the study.
To consider ethical principles, the objectives of the study were explained to the participants, and they were ensured about the confidentiality of their information. They signed a written informed consent form and were free to leave the study at any time.
The data collection tools were a demographic form, Mini Nutritional Assessment (MNA), and the General Health Questionnaire (GHQ). They were completed by the researcher through the interview with participants. The MNA is a simple, low-cost, non-invasive method that can be performed at the bedside. It is a useful screening tool for diagnosing malnutrition and the risk of malnutrition in the elderly. It consists of 18 items and anthropometric indicators to rank the subjects at three levels of malnourished (total score <17), at risk of malnutrition (total scores of 17-23.5), and normal nutritional status (total scores of 24-30) [18].
The MNA questions are divided into four categories of anthropometric indices, general condition, eating patterns, and self-perceived nutrition/health. The surveyed information is about declined food intake, weight loss greater than 3 kg, mobility, bound to bed or chair, psychological stress, neuropsychological problems, Body Mass Index (BMI), inability to live independently, taking more than three prescription drugs, having pressure sores or skin ulcers, number of full meals per day, high-protein food intake, consumption of fruits and vegetables, amount of liquids consumed daily, inability to self-feed, self-feeding with difficulty, self-perception of nutritional status, self-perception of health status, Mid-Arm Circumference (MAC), and Calf Circumference (CC) [19, 20]. In the present study, the Cronbach alpha coefficient for MNA was obtained at 0.83.
The GHQ has 12 items, 6 positive and 6 negative ones. The items are rated on a 4-point scale from “never” to “always”. There are two scoring styles for this questionnaire, bimodal (0-0-1-1) and Rating-type (0-1-2-3) method. We used the bimodal scoring method. The score >3.7 shows undesirable general health [21-23].
The demographic form collected the information on gender, age, weight, height, and body mass index and history of diseases. Based on BMI, the participants were divided into four groups of lean (BMI <20), normal (BMI=20-26), overweight (BMI=26-30), and obese (BMI >30) [24]. History of diseases was examined using their medical records.
The body weight was measured by two trained individuals using a digital scale (SECA model), while the participants were with light clothing and no shoes; for the body height measurement, an inelastic stadiometer with an accuracy of 0.5cm was used. Mid-arm circumference and calf circumference of participants were also measured. Moreover, BMI was estimated by dividing the weight in kilograms by the height in meters squared. The collected data were analyzed in SPSS V. 22. The Kolmogorov-Smirnov test was used to investigate the normal distribution of the study variables. Descriptive statistics and Spearman correlation coefficient, independent t-test, and one way ANOVA were used for analyzing data. The significance level was set as P=0.05.
Results
Of 184 participants, 113(66.2%) were female and 71 (33.8%) male. Their Mean±SD age was 68.9±7.8 year. The Mean±SD MNA score was reported 20.9±2.7 in men and 20.9±3.6 in women, and based on t-test results, and there was no significant difference between groups. About (19.2%) had malnutrition (Mean±SD= 15.1±1.20), (52.17%) were at risk of developing malnutrition (Mean±SD=20.4±1.9), and (28.8%) had normal nutritional state (Mean±SD=24.7±9). Table 1 presents the nutritional status of the participants based on gender.
alnutrition is usually defined as a faulty or bad nutritional status, which has adverse effects on the health and the quality of life of the older people [1]. In addition, it imposes a high cost on health care systems [2]. Malnutrition is an essential component of geriatric care [1]. Older people are vulnerable to malnutrition, and it is one of the common problems in this age group [3, 4]. Its prevalence in healthy older people is (5-10%), in older patients (30-60%), and in older people living in nursing homes (2-74%) depending on the assessment method [4]. In Iran, the prevalence of malnutrition has been reported (9.2%) among older people living independently and (26.1%) among those living in nursing homes [5]. Recent studies have identified several predisposing factors for malnutrition in older people, including demographic characteristics, economic conditions, diet, appetite, disease, social factors, and healthy behaviors [1, 6]. Inadequate nutritional status predisposes older people to develop diseases such as osteoporosis, diabetes, cardiovascular disease, and high blood pressure and incur higher health costs [7].
On the other hand, these people usually suffer from one or more diseases at the same time, and recent studies have reported the prevalence of multimorbidity in the elderly as (56-67%) [8-10]. Malnutrition is crucial both for the health system and for the patient as it reduces the quality of life, causes longer stay in hospital and higher costs and mortality rate [11, 12]. The presence of various diseases in older people and their poor general health status are effective and predictors of malnutrition [13-15]. According to studies conducted in Iran, the general health status of older people is moderate or undesirable. One study reported that (61.7%) of them had a poor health status [16]. Despite the growth of the elderly population in Iran and change in the population pyramid, less attention has been paid to the general health status of older people as a vulnerable group [17].
Regarding what was discussed, the study of nutritional status in older people living in nursing homes in order to identify general problems and factors associated with their malnutrition can enrich our knowledge about the aging and its threatening factors. On the other hand, providing health and identifying the needs of the elderly requires a comprehensive and accurate understanding of their health status. Furthermore, considering the aging of the population in the future, the prevalence of malnutrition among older people, and particularly in nursing homes, it is crucial to pay more attention to this issue [5]. By studying the relationship between nutritional status, general health, and multimorbidity, it is possible to design interventions to influence factors associated with malnutrition and thus reduce its prevalence. A few studies have evaluated the prevalence of malnutrition concerning general health and multimorbidity among older people in Iran. In this regard, this study aimed to assess this issue among older people living in nursing homes of Ahvaz City, Iran.
Materials and Methods
This is an analytical cross-sectional study. Study population consisted of all 250 older people living in 4 nursing homes in Ahvaz City, who were selected using the census method and met the inclusion criteria as follows: able to speak; informed consent to participate in the study; age >60 years; no Alzheimer disease, memory impairment, or dementia (according to the medical records); and not participating in other studies. The exclusion criterion was their unwillingness to continue the study. Based on these criteria, 184 older people were entered into the study.
To consider ethical principles, the objectives of the study were explained to the participants, and they were ensured about the confidentiality of their information. They signed a written informed consent form and were free to leave the study at any time.
The data collection tools were a demographic form, Mini Nutritional Assessment (MNA), and the General Health Questionnaire (GHQ). They were completed by the researcher through the interview with participants. The MNA is a simple, low-cost, non-invasive method that can be performed at the bedside. It is a useful screening tool for diagnosing malnutrition and the risk of malnutrition in the elderly. It consists of 18 items and anthropometric indicators to rank the subjects at three levels of malnourished (total score <17), at risk of malnutrition (total scores of 17-23.5), and normal nutritional status (total scores of 24-30) [18].
The MNA questions are divided into four categories of anthropometric indices, general condition, eating patterns, and self-perceived nutrition/health. The surveyed information is about declined food intake, weight loss greater than 3 kg, mobility, bound to bed or chair, psychological stress, neuropsychological problems, Body Mass Index (BMI), inability to live independently, taking more than three prescription drugs, having pressure sores or skin ulcers, number of full meals per day, high-protein food intake, consumption of fruits and vegetables, amount of liquids consumed daily, inability to self-feed, self-feeding with difficulty, self-perception of nutritional status, self-perception of health status, Mid-Arm Circumference (MAC), and Calf Circumference (CC) [19, 20]. In the present study, the Cronbach alpha coefficient for MNA was obtained at 0.83.
The GHQ has 12 items, 6 positive and 6 negative ones. The items are rated on a 4-point scale from “never” to “always”. There are two scoring styles for this questionnaire, bimodal (0-0-1-1) and Rating-type (0-1-2-3) method. We used the bimodal scoring method. The score >3.7 shows undesirable general health [21-23].
The demographic form collected the information on gender, age, weight, height, and body mass index and history of diseases. Based on BMI, the participants were divided into four groups of lean (BMI <20), normal (BMI=20-26), overweight (BMI=26-30), and obese (BMI >30) [24]. History of diseases was examined using their medical records.
The body weight was measured by two trained individuals using a digital scale (SECA model), while the participants were with light clothing and no shoes; for the body height measurement, an inelastic stadiometer with an accuracy of 0.5cm was used. Mid-arm circumference and calf circumference of participants were also measured. Moreover, BMI was estimated by dividing the weight in kilograms by the height in meters squared. The collected data were analyzed in SPSS V. 22. The Kolmogorov-Smirnov test was used to investigate the normal distribution of the study variables. Descriptive statistics and Spearman correlation coefficient, independent t-test, and one way ANOVA were used for analyzing data. The significance level was set as P=0.05.
Results
Of 184 participants, 113(66.2%) were female and 71 (33.8%) male. Their Mean±SD age was 68.9±7.8 year. The Mean±SD MNA score was reported 20.9±2.7 in men and 20.9±3.6 in women, and based on t-test results, and there was no significant difference between groups. About (19.2%) had malnutrition (Mean±SD= 15.1±1.20), (52.17%) were at risk of developing malnutrition (Mean±SD=20.4±1.9), and (28.8%) had normal nutritional state (Mean±SD=24.7±9). Table 1 presents the nutritional status of the participants based on gender.
The MNA scores showed that (86.2%) of the participants were taking more than three prescription drugs; (26.4%) suffered from psychological stress or acute disease in the past three months; (58.5%) considered their health status worse than others, and (29.2%) did not know about it. Also, (20.8%) had pressure sores or skin ulcers; (40%) were bed- or chair-bound; (20%)had self-perception of being malnourished, and (41.5%)were uncertain of their nutritional state. None of them had weight loss greater than three kg during the last three months. About (32.2%) had neuropsychological problems, and (19.2%) had one full meal per day. Around (30%) had fruits and vegetables less than two times per day, and (29.2%) drank liquids less than three cups per day. Of them, (37.7%) were unable to eat without assistance, and (30.8%) had reduced food intake due to loss of appetite.
To examine the correlation between variables, the Spearman correlation test was carried out. The results showed that MNA score had a significant correlation with reduced food intake (r=0.56, P=0.001), mobility (r=0.60, P=0.001), BMI (r=0.43, P=0.001), and neuropsychological problems (r=0.37, P=0.001). Moreover, there was a significant relationship between BMI and inability to live independently (r=-0.24, P=0.006), also between BMI and MAC (r=0.48, P=0.001), and between high-protein food intake and CC (r=0.26, P=0.003) and between high-protein food intake and skin problems (r=0.71, P<0.001). Regarding multimorbidity status, (5%) had no disease, (24%) one disease, (36%) two diseases, and (35%) three or more and. Among the diseases that subjects were suffering from, depression was the most common disease (62.8%) followed by cardiovascular disease (47%) and joint pain (44.6%). The Mean±SD of nutritional state in subjects with depression was 20.44±3.37 and in non-depressed ones, it was 21.79±3.07 indicating the poorer nutritional status of the elderly with depression (P=0.02). Comparing the nutritional status with the type of disease showed no significant relationship between them.
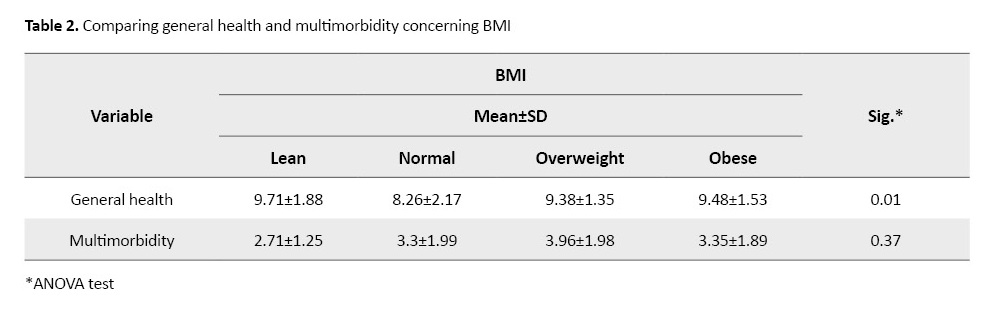
The Mean±SD GHQ score was reported 9.26±1.7 ranging from 0-12. A total of 182 (99.26%) samples had undesirable general health status (GHQ score >3.5). There was no statistically significant relationship between general health and malnutrition. The comparison of general health status based on BMI showed that the most favorable general health status was related to the elderly group with normal BMI, and other BMI groups had a lower general health status (P=0.01). In comparing the relationship between multimorbidity and BMI, it was found that with the increase in BMI, the multimorbidity level increased; however, the mean difference was not statistically significant (Table 2).
To examine the correlation between variables, the Spearman correlation test was carried out. The results showed that MNA score had a significant correlation with reduced food intake (r=0.56, P=0.001), mobility (r=0.60, P=0.001), BMI (r=0.43, P=0.001), and neuropsychological problems (r=0.37, P=0.001). Moreover, there was a significant relationship between BMI and inability to live independently (r=-0.24, P=0.006), also between BMI and MAC (r=0.48, P=0.001), and between high-protein food intake and CC (r=0.26, P=0.003) and between high-protein food intake and skin problems (r=0.71, P<0.001). Regarding multimorbidity status, (5%) had no disease, (24%) one disease, (36%) two diseases, and (35%) three or more and. Among the diseases that subjects were suffering from, depression was the most common disease (62.8%) followed by cardiovascular disease (47%) and joint pain (44.6%). The Mean±SD of nutritional state in subjects with depression was 20.44±3.37 and in non-depressed ones, it was 21.79±3.07 indicating the poorer nutritional status of the elderly with depression (P=0.02). Comparing the nutritional status with the type of disease showed no significant relationship between them.
The Mean±SD GHQ score was reported 9.26±1.7 ranging from 0-12. A total of 182 (99.26%) samples had undesirable general health status (GHQ score >3.5). There was no statistically significant relationship between general health and malnutrition. The comparison of general health status based on BMI showed that the most favorable general health status was related to the elderly group with normal BMI, and other BMI groups had a lower general health status (P=0.01). In comparing the relationship between multimorbidity and BMI, it was found that with the increase in BMI, the multimorbidity level increased; however, the mean difference was not statistically significant (Table 2).
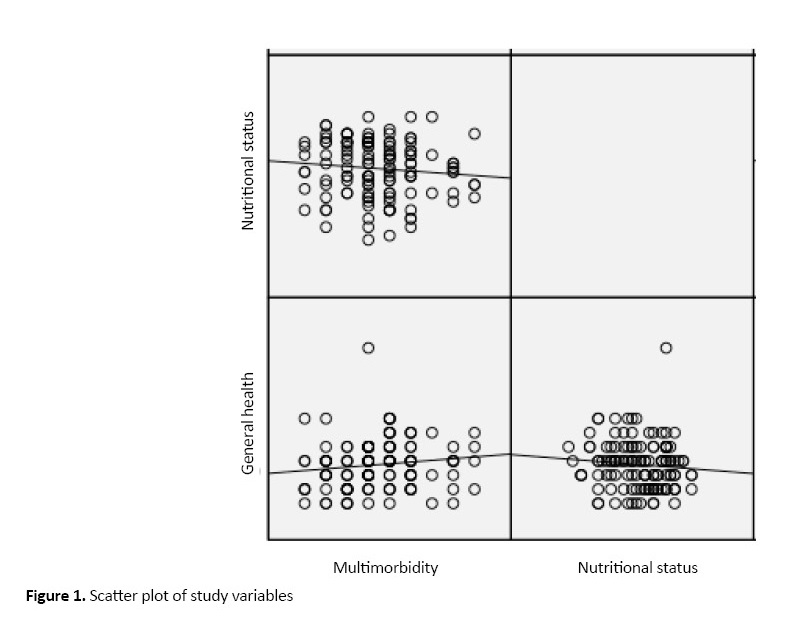
Regarding the association between general health and multimorbidity, the results revealed a significant positive association (r=0.92, P=0.02). Considering that higher scores represent lower general health level, with the increase in multimorbidity, the general health score increased, and as a result, the general health condition became more unfavorable. The correlation of nutritional status with multimorbidity and general health was not statistically significant. Figure 1 presents the scatter plot of study variables.
Discussion
The study showed that a high percentage of older people living in nursing homes were malnourished or at risk of malnutrition. The health status of the residents was undesirable, too, and more than two-thirds of them had three or more diseases. These results are consistent with the results of Konda et al. in India [18]. In their study, (9.1%) of the samples were malnourished, and (32.5%) were at risk of malnutrition. The difference in the prevalence rate between ours and their study may be related to the difference in the study area. Moreover, their study was conducted on older people in the general population, while our study was conducted on the elderly residents of nursing homes. Shivraj et al. also reported the undesirable nutritional status of older people in their research [25].
Based on the findings of this study, the undesirable nutritional status in the elderly residents of nursing homes was high and considerable. Comparing the nutritional status of older people living in their own houses with that of the elderly living in nursing homes, various studies have shown that malnutrition in the elderly residents of nursing homes is more prevalent than in those living with their families [15, 26]. In this case, it can be said that nutritional status in the elderly is affected by various cultural, social, economic, and health conditions. On the other hand, the high prevalence of malnutrition among the elderly living in nursing homes can be due to social deprivations and loneliness [27]. Other factors can also be involved, including the type of food, limitation in doing delicate tasks such as grasping a spoon, concurrent use of medications, and food composition [28]. Because of this inability and the need for care or assistance, a high prevalence of malnutrition among older residents is not surprising [4].
Regarding the undesirable general health status of the elderly in our study, it is in agreement with the results of Maghsoudi and associates [16]. This finding can be explained by older people’s residing in the nursing home care, that changes their past social relationships losing their support previously received from the family [29]. This change may result in a reduction in their general health in various dimensions.
In our study, more than one-third of the samples had three or more diseases, most commonly depression, cardiovascular disease, and joint pain. The study results indicate that the prevalence of multimorbidity among older people is (20-60%) [12, 30, 31]. However, our result is consistent with the results of Doumit and Nasser and Pilania et al. The high prevalence of depression among the elderly, especially those living in nursing homes, can be due to loneliness and separation from the family [32, 33].
Our results also showed no significant relationship between nutritional status and general health of the elderly residents, and with the increase of nutritional status score, their general health score decreased. According to the scoring style of GHQ questionnaire, lower scores indicate a better level of general health [21]. Thus, any improvement in nutritional status will improve the general health level of older people. Possibly, the non-significant relationship between these two variables may be due to the low sample size of the study. Therefore, it is recommended to use a larger sample size in future studies. In the present study, a significant positive relationship was found between general health and multimorbidity. The presence of various diseases in the elderly influences cognitive functions, causes depression, and reduces mobility in them, and thus lowers their general health [34-36]. Since with the increase of age, the risk of chronic diseases in the elderly increases, it is necessary to pay attention to the supportive factors and other underlying variables to empower them so that their general health be promoted.
Among the various diseases reported by the elderly in our study, depression was significantly associated with the MNA score, which is consistent with the results of Otte [37]. Cognitive impairments in older people seem to affect their functional status and physical activity, which cause reduced food intake and loss of appetite. Bailly et al. stated that physical, psychological, and social factors such as living alone, low social and economic status, the individual’s view of health, and disability affect depression, which in turn decline the nutritional status of the elderly [38].
In our study, we found a significant positive correlation between the MNA score and BMI of the elderly, which is in agreement with the results of Soini and Routasalo [39]. The general health of the participants was also significantly correlated with BMI. The BMI of women was higher than that of men. Meenu et al. also reported a higher BMI in women [40]. Naturally, body fat in women is more than men, and women are less involved in physical mobility, which increase the likelihood of women’s being overweight and obese.
One of the limitations of this study was the non-generalizability of the results to the all Iranian aging population. Given the high prevalence of poor nutritional status and general health in the elderly living in nursing homes, it seems that, in addition to dietary interventions for this group, it is essential to provide the necessary facilities for their social and economic support and training the nursing staff of elderly care centers. The high prevalence of depression among residents of nursing homes and its relationship with nutritional status is noticeable, too. In this regard, it is recommended that other interventional studies, the presence of psychologists in nursing homes, educating caregivers, controlling the causes of depression and considering other psychological aspects of life in nursing homes be conducted and taken into account.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Ahvaz University of Medical Sciences (Code: IR.AJUMS.REC.1394.508).
Funding
The Deputy for Research of Ahvaz University of Medical Sciences financial supported this study with the registered project No. SDH-9416.
Authors contributions
Conceptualization, proposal: Shahab Papi, Marzie Zilaee, Parvin Shahry; Investigation, Writing-original draft: Parvin Shahry,Shahab Papi, Marzie Zilaee, Marzie Zilaee.
Conflict of interest
The authors declared no conflict of interests.
Acknowledgements
The authors would like to thank the management and elderly residents of study nursing homes for their valuable cooperation.
References
The study showed that a high percentage of older people living in nursing homes were malnourished or at risk of malnutrition. The health status of the residents was undesirable, too, and more than two-thirds of them had three or more diseases. These results are consistent with the results of Konda et al. in India [18]. In their study, (9.1%) of the samples were malnourished, and (32.5%) were at risk of malnutrition. The difference in the prevalence rate between ours and their study may be related to the difference in the study area. Moreover, their study was conducted on older people in the general population, while our study was conducted on the elderly residents of nursing homes. Shivraj et al. also reported the undesirable nutritional status of older people in their research [25].
Based on the findings of this study, the undesirable nutritional status in the elderly residents of nursing homes was high and considerable. Comparing the nutritional status of older people living in their own houses with that of the elderly living in nursing homes, various studies have shown that malnutrition in the elderly residents of nursing homes is more prevalent than in those living with their families [15, 26]. In this case, it can be said that nutritional status in the elderly is affected by various cultural, social, economic, and health conditions. On the other hand, the high prevalence of malnutrition among the elderly living in nursing homes can be due to social deprivations and loneliness [27]. Other factors can also be involved, including the type of food, limitation in doing delicate tasks such as grasping a spoon, concurrent use of medications, and food composition [28]. Because of this inability and the need for care or assistance, a high prevalence of malnutrition among older residents is not surprising [4].
Regarding the undesirable general health status of the elderly in our study, it is in agreement with the results of Maghsoudi and associates [16]. This finding can be explained by older people’s residing in the nursing home care, that changes their past social relationships losing their support previously received from the family [29]. This change may result in a reduction in their general health in various dimensions.
In our study, more than one-third of the samples had three or more diseases, most commonly depression, cardiovascular disease, and joint pain. The study results indicate that the prevalence of multimorbidity among older people is (20-60%) [12, 30, 31]. However, our result is consistent with the results of Doumit and Nasser and Pilania et al. The high prevalence of depression among the elderly, especially those living in nursing homes, can be due to loneliness and separation from the family [32, 33].
Our results also showed no significant relationship between nutritional status and general health of the elderly residents, and with the increase of nutritional status score, their general health score decreased. According to the scoring style of GHQ questionnaire, lower scores indicate a better level of general health [21]. Thus, any improvement in nutritional status will improve the general health level of older people. Possibly, the non-significant relationship between these two variables may be due to the low sample size of the study. Therefore, it is recommended to use a larger sample size in future studies. In the present study, a significant positive relationship was found between general health and multimorbidity. The presence of various diseases in the elderly influences cognitive functions, causes depression, and reduces mobility in them, and thus lowers their general health [34-36]. Since with the increase of age, the risk of chronic diseases in the elderly increases, it is necessary to pay attention to the supportive factors and other underlying variables to empower them so that their general health be promoted.
Among the various diseases reported by the elderly in our study, depression was significantly associated with the MNA score, which is consistent with the results of Otte [37]. Cognitive impairments in older people seem to affect their functional status and physical activity, which cause reduced food intake and loss of appetite. Bailly et al. stated that physical, psychological, and social factors such as living alone, low social and economic status, the individual’s view of health, and disability affect depression, which in turn decline the nutritional status of the elderly [38].
In our study, we found a significant positive correlation between the MNA score and BMI of the elderly, which is in agreement with the results of Soini and Routasalo [39]. The general health of the participants was also significantly correlated with BMI. The BMI of women was higher than that of men. Meenu et al. also reported a higher BMI in women [40]. Naturally, body fat in women is more than men, and women are less involved in physical mobility, which increase the likelihood of women’s being overweight and obese.
One of the limitations of this study was the non-generalizability of the results to the all Iranian aging population. Given the high prevalence of poor nutritional status and general health in the elderly living in nursing homes, it seems that, in addition to dietary interventions for this group, it is essential to provide the necessary facilities for their social and economic support and training the nursing staff of elderly care centers. The high prevalence of depression among residents of nursing homes and its relationship with nutritional status is noticeable, too. In this regard, it is recommended that other interventional studies, the presence of psychologists in nursing homes, educating caregivers, controlling the causes of depression and considering other psychological aspects of life in nursing homes be conducted and taken into account.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Ahvaz University of Medical Sciences (Code: IR.AJUMS.REC.1394.508).
Funding
The Deputy for Research of Ahvaz University of Medical Sciences financial supported this study with the registered project No. SDH-9416.
Authors contributions
Conceptualization, proposal: Shahab Papi, Marzie Zilaee, Parvin Shahry; Investigation, Writing-original draft: Parvin Shahry,Shahab Papi, Marzie Zilaee, Marzie Zilaee.
Conflict of interest
The authors declared no conflict of interests.
Acknowledgements
The authors would like to thank the management and elderly residents of study nursing homes for their valuable cooperation.
References
- Damayanthi H, Moy F, Abdullah K, Dharmaratne SJB. Prevalence of malnutrition and associated factors among community-dwelling older persons in Sri Lanka: A cross-sectional study. BMC Geriatrics. 2018; 18:199. [DOI:10.1186/s12877-018-0892-2] [PMID] [PMCID]
- Leslie W, Hankey C. Aging, nutritional status and health. Healthcare. 2015; 3(3):648-58. [DOI:10.3390/healthcare3030648] [PMID] [PMCID]
- World Health Organization. Active ageing: A policy framework. Geneva: World Health Organization; 2002.
- Başibüyük Gö, Ayremlou P, Saeidlou Sn, Çinar Z, Aye F, Bektaş Y, et al. Evaluation of malnutrition among elderly people living in nursing homes by Mini Nutritional Assessment Short Form (MNA-SF) in Turkey. Maedica A Journal of Clinical Medicine. 2019; 14(1):38-44. [PMID] [PMCID]
- Gorji HA, Alikhani M, Mohseni M, Moradi-Joo M, Ziaiifar H, Moosavi A. The prevalence of malnutrition in Iranian elderly: A review article. Iranian Journal of Public Health. 2017; 46(12):1603-10. [PMID] [PMCID]
- Niknami M, Namjoo A, Baghaee M, Sedghei Sabet M, Atrkar Roshan Z. [Survey healthbehavior of elderly referring to retirement centers in Rasht city in 20% (Persian)]. Journal of Holistic Nursing and Midwifery. 2010; 20(1):40-8.
- Taylor C. Malnutrition: Causes, consequences and solutions. Journal of Community Nursing. 2018; 32(6):52-6.
- Ruiz M, Bottle A, Long S, Aylin PJ. Multi-morbidity in hospitalised older patients: Who are the complex elderly? PLOS One. 2015; 10(12):e0145372. [DOI:10.1371/journal.pone.0145372] [PMID] [PMCID]
- Jovic D, Vukovic D, Marinkovic JJ. Prevalence and patterns of multi-morbidity in Serbian adults: A cross-sectional study. PLOS One. 2016; 11(2):e0148646. [DOI:10.1371/journal.pone.0148646] [PMID] [PMCID]
- Van den Akker M, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA. Multimorbidity in general practice: Prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. Journal of Clinical Epidemiology. 1998; 51(5):367-75. [DOI:10.1016/S0895-4356(97)00306-5]
- Williams JS, Egede LE. The association between multimorbidity and quality of life, health status and functional disability. The American Journal of the Medical Sciences. 2016; 352(1):45-52. [DOI:10.1016/j.amjms.2016.03.004] [PMID]
- Park B, Ock M, Lee HA, Lee S, Han H, Jo MW, et al. Multimorbidity and health-related quality of life in Koreans aged 50 or older using KNHANES 2013-2014. Health and Quality of Life Outcomes. 2018; 16:186. [DOI:10.1186/s12955-018-1016-6] [PMID] [PMCID]
- Shi R, Duan J, Deng Y, Tu Q, Cao Y, Zhang M, et al. Nutritional status of an elderly population in southwest China: A cross-sectional study based on comprehensive geriatric assessment. The Journal of Nutrition, Health & Aging. 2015; 19(1):26-32. [DOI:10.1007/s12603-014-0471-y] [PMID]
- Vanderwee K, Clays E, Bocquaert I, Gobert M, Folens B, Defloor T. Malnutrition and associated factors in elderly hospital patients: A Belgian cross-sectional, multi-centre study. Clinical Nutrition. 2010; 29(4):469-76. [DOI:10.1016/j.clnu.2009.12.013] [PMID]
- Wei JM, Li S, Claytor L, Partridge J, Goates S. Prevalence and predictors of malnutrition in elderly Chinese adults: Results from the China health and retirement longitudinal study. Public Health Nutrition. 2018; 21(17):3129-34. [DOI:10.1017/S1368980018002227] [PMID] [PMCID]
- Maghsoudi A, Dindarloo S, Jamali T, Ghaed S, Rastgoo Z, Hassanipour AS. [Comparison of sleep quality and general health in elderly individuals living in their houses and nursing homes (Persian)]. Sadra Medical Sciences Journal. 2017; 4(3)161-71.
- Tohidi M, Halantarhormozi M, Adinehpoor A, Dabbaghmanesh M, Siadatian J, Ranjbar Omrani G. Prevalence of overweight and obesity in adults in Shiraz-2009. Iranian Journal of Diabetes and Metabolism. 2010; 9:43-8.
- Konda S, Giri PA. Prevalence of malnutrition and its determinants in an elderly people in South India. International Journal of Community Medicine and Public Health. 2018; 5(8):3570-6. [DOI:10.18203/2394-6040.ijcmph20183100]
- Gazzotti C, Arnaud‐Battandier F, Parello M, Farine S, Seidel L, Albert A, et al. Prevention of malnutrition in older people during and after hospitalisation: Results from a randomised controlled clinical trial. Age and Ageing. 2003; 32(3):321-5. [DOI:10.1093/ageing/32.3.321] [PMID]
- Masomy N, Jefroodi S, Ghanbari A, Kazemnejad E, Shojaei F, Rafiei A. [Nutritional status assessment and related factors in the retired senile (Persian)]. Journal of Guilan University of Medical Sciences. 2012; 21(84):65-70.
- Dehghankar L, Shahrokhi A, Qolizadeh A, Mohammadi F, Nasiri E. Health promoting behaviors and general health among the elderly in Qazvin: A cross sectional study. Elderly Health Journal. 2018; 4(1):18-22.
- Ebadi M, Harir CA, Shariati M, Garmaroudi Gh, Fateh A, Montazeri A. [Translation, reliability and validity of the 12-item general health questionnaire among young people in Iran (Persian)]. Payesh. 2002; 1(3):39-46.
- Yaghubi H, Karimi M, Omidi A, Barooti E, Abedi M. [Validity and factor structure of the General Health Questionnaire (GHQ-12) in university students (Persian)]. International Journal of Behavioral Sciences. 2012; 6(2):153-60.
- Khezry A, Arab Ameri E, R H. [The effect of body mass index on the reaction time and response of active and inactive elderly (Persian)]. Journal of Behavioral Movement and Psychology of Exercise. 2014; 6(1):1-21.
- Shivraj M, Singh V, Meena B, Kusum S, Neelam M, Dayal S. Study of nutritional status in elderly in Indian population. International Journal of Current Research. 2014; 6(11):10253-7.
- Bolmsjö BB, Jakobsson U, Mölstad S, Östgren CJ, Midlöv P. The nutritional situation in Swedish nursing homes, a longitudinal study. Archives of Gerontology and Geriatrics. 2015; 60(1):128-33. [DOI:10.1016/j.archger.2014.10.021] [PMID]
- Volkert D, Frauenrath C, Kruse W, Oster P, Schlierf G. Malnutrition in old age-results of the Bethany nutrition study. Therapeutische Umschau. Revue Therapeutique. 1991; 48(5):312-5.
- Ghasemi S, Sharifi F, Maghsoodnia S, Teymoori F. [The effect of health - nutrition education on health promotion in resident elderly in Kahrizak in Tehran (Persian)]. Salmand. 2006; 1(1):34-45.
- Lee DT. Transition to residential care: Experiences of elderly Chinese people in Hong Kong. Journal of Advanced Nursing. 1999; 30(5):1118-26. [DOI:10.1046/j.1365-2648.1999.01196.x] [PMID]
- Orueta JF, García-Álvarez A, García-Goñi M, Paolucci F, Nuño-Solinís RJ. Prevalence and costs of multimorbidity by deprivation levels in the Basque Country: A population based study using health administrative databases. PLOS One. 2014; 9(2):e89787. [DOI:10.1371/journal.pone.0089787] [PMID] [PMCID]
- Roberts KC, Rao DP, Bennett TL, Loukine L, Jayaraman GC. Prevalence and patterns of chronic disease multimorbidity and associated determinants in Canada. Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice. 2015; 35(6):87-94. [DOI:10.24095/hpcdp.35.6.01] [PMID] [PMCID]
- Doumit J, Nasser R. Quality of life and wellbeing of the elderly in Lebanese nursing homes. International Journal of Health Care Quality Assurance. 2010; 23(1):72-93. [DOI:10.1108/09526861011010695] [PMID]
- Pilania M, Yadav V, Bairwa M, Behera P, Gupta SD, Khurana H, et al. Prevalence of depression among the elderly (60 years and above) population in India, 1997-2016: A systematic review and meta-analysis. BMC Public Health. 2019; 19:832. [DOI:10.1186/s12889-019-7136-z] [PMID] [PMCID]
- Moodi M, Sharifzadeh G, Saadatjoo SS. General health status and its relationship with health-promoting lifestyle among patients with hypertension. Modern Care Journal. 2015; 12(4):e8674. [DOI:10.17795/modernc.8674]
- Nourdini A, Jouybari L, Sanagoo A, Kavosi A. Public health, life satisfaction and quality of life of elderly patients with coronary artery disease admitted to hospitals Nursing. Development in Health. 2016; 7(1):31-40.
- Papi S, Karimi Z, Ghaed Amini Harooni G, Nazarpour A, Shahry P. Determining the prevalence of sleep disorder and its predictors among elderly residents of nursing homes of Ahvaz city in 2017. Iranian Journal of Ageing. 2019; 13(5):576-87. [DOI:10.32598/SIJA.13.Special-Issue.576]
- Otte C. Incomplete remission in depression: Role of psychiatric and somatic comorbidity. Dialogues in Clinical Neuroscience. 2008; 10(4):453-60.
- Bailly N, Maître I, Van Wymelbeke V. Relationships between nutritional status, depression and pleasure of eating in aging men and women. Archives of Gerontology and Geriatrics. 2015; 61(3):330-6. [DOI:10.1016/j.archger.2015.08.020] [PMID]
- Soini H, Routasalo P, Lagström H. Characteristics of the Mini-Nutritional assessment in elderly home-care patients. European Journal of Clinical Nutrition. 2004; 58(1):64-70. [DOI:10.1038/sj.ejcn.1601748] [PMID]
- Kalia M, Virk A, Gupta BP, Singh J. Assessment of malnourishment in elderly of rural Punjab. Healthline. 2014; 5(2):24-8.
Article Type : Research |
Subject:
General
Received: 2019/07/4 | Accepted: 2019/08/10 | Published: 2019/10/1
Received: 2019/07/4 | Accepted: 2019/08/10 | Published: 2019/10/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |